With millions of cases around the world, our understanding of the acute illness caused by Covid-19 has improved enormously. But it is now clear that large numbers of people infected by the virus are experiencing symptoms that can go on for months. Charles Bangham, Professor of Immunology at Imperial College London, looks at what we know about the long-term effects of Covid-19 and just how long they might last.
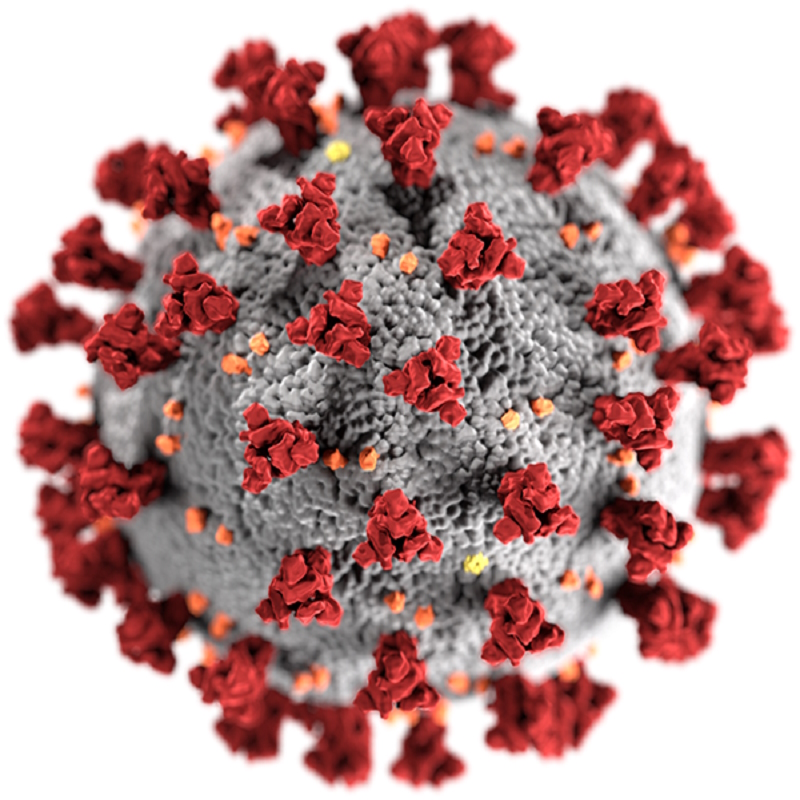
Most people who catch the coronavirus SARS-CoV-2 are either asymptomatic or have only a mild illness. If symptoms of Covid-19 develop, they typically appear within 2-14 days of being infected and last for a couple of weeks. Sadly, around 1% of those who catch the SARS-CoV-2 virus die. Fortunately, as we have got better at treating severe cases, survival rates are improving.
But as the pandemic enters its second year, it is now clear that beating an initial infection from this virus is not the end of the story. For a significant proportion of people, Covid-19 is turning out to be a long-term illness – a condition that has become known as “Long Covid”.
For weeks and even months after the initial infection is thought to subside, patients are reporting a wide range of persistent symptoms. According to some estimates, between 2.3% and 10% of people who test positive for Covid-19 experience some symptoms for 12 weeks or longer. These can include fatigue, breathlessness, headaches, chest pains, palpitations and dizziness. Yet, there still isn’t a clear idea of just how common Long Covid is or how serious a problem it is likely to be, both for individual patients and wider society as a whole.
A major part of the problem is that we still do not have a widely accepted definition of exactly what Long Covid is. To even begin to estimate how much of a problem the condition is, we need to have a clear idea of how to identify it.
Part of the reason for this is the newness of Covid-19 itself; the disease was only recognised in December 2019 and has been in some countries for less than a year. The long-term effects started to be recognised in the summer of 2020 as the numbers suffering then grew.
Initially Long Covid was sometimes described as being symptoms that lasted for longer than four weeks. At the end of 2020, however, the National Institute for Health and Care Excellence (NICE) took a step towards a better definition. Its guidelines stated that Covid-19 itself can last up to four weeks, and persistent symptoms lasting 4-12 weeks were described as “ongoing symptomatic Covid-19”. Symptoms that persisted 12 weeks or more were classed as “post-Covid-19 syndrome”.
Even so, there are still nearly 50 different symptoms associated with Long Covid and some surveys have identified more than 100. Yet the most frequently reported symptoms are fairly non-specific – headaches, fatigue and breathlessness, for example, are common in many different conditions. Not everyone experiences all of the symptoms in the same combinations, and in some cases they appear intermittently. Often the symptoms change over time and appear in different parts of the body. This all makes it hard for doctors to ascribe it to a single condition.
Long Covid has also been largely neglected as an area of research so far in the pandemic. Rightly, clinicians and scientists have focused their attention on dealing with the more immediate acute disease. Initially there was also a tendency for cases to be put down as having a psychosomatic cause – perhaps due to the stress or anxiety caused by a Covid-19 infection. It is a response that has frustrated those – healthcare professionals among them – living through the experience of Long Covid.
It is now apparent that Long Covid is far too common to be wholly due to psychosomatic factors. But it is still unclear whether there is one underlying mechanism of Long Covid, or whether it is a collection of different conditions. If we were to use Occam's Razor – that is, that often the simplest explanation is the best route to the truth – it is clear that infection with Covid-19 is a necessary precipitating cause. What additional role pre-existing conditions and genetics play have still to be established.
But to really understand what is going on, it will be necessary to find an underlying mechanism for how the virus is causing this wide collection of long lasting symptoms and signs.
There are a couple of possible explanations – first the virus itself could be hiding in the body, much like we see with the Epstein Barr virus (EBV) that causes glandular fever, and herpes viruses that can hide in the body in a latent state before reactivating. Alternatively, Long Covid could be the result of a persistent immune response triggered by the virus that then causes inflammation and damage to other parts of the body. Finally, it could be due to tissue damage done during the acute phase of the illness.
For example, we know that one of the cell types that SARS-COV-2 is able to infect is the lining of blood vessels, and one of the serious problems in acute Covid-19 is widespread blood clotting. So one possibility is that a combination of damage to the lining of small blood vessels and abnormal blood clotting could affect the blood supply to different organs, causing heart disease in one person and a stroke in another person. This could explain why we see so many different manifestations of Long Covid, although I must emphasise this is just one possibility – we need good evidence to find out what is really going on.
There have been comparisons, however, between Long Covid and another condition that is often linked to viral infections – chronic fatigue syndrome (CFS), also sometimes called post-viral fatigue or ME. While the cause of CFS is the source of controversy in some circles, there could be wider lessons to be learned from Long Covid for the medical community. If we can understand how Long Covid is caused, we might gain a better understanding of how chronic fatigue can follow some other viral infections.
Unravelling the cause of Long Covid will not only make it easier to diagnose people suffering from this debilitating condition, but also help us to start doing something about it too.
Currently the only treatments available are those that manage the symptoms and encourage patients to look after their general health through diet, rest and exercise. Until more is known about how an infection with Covid-19 can lead to long-term symptoms, it will be difficult to do more.
Another key question weighing on the minds of those currently wrestling with Long Covid is how long they are likely to continue suffering. For health professionals and systems around the world, it is an important one to answer too as treating patients with Long Covid is likely to require more and more resources as the number of infections continue to grow. In the UK, the NHS has already spent £10 million setting up a network of Long Covid clinics around the country to offer specialist help to those with long term symptoms from Covid-19. For some – even those who have had mild to moderate cases of Covid-19 – the road to recovery is proving to be a slow, painful one.
In July last year, Paul Garner, a professor of epidemiology at Liverpool School of Tropical Medicine, described how 95 days after the onset of Covid-19 he still found himself unable to get out of bed for more than three hours at a time, he suffered from pain in his arms and legs, experienced palpitations and was addled with brain fog. By September – six months since his initial infection – he was still suffering.
His story seems common among those who share details of their experience with Long Covid. One survey involving 3,700 patients found that people were still suffering symptoms up to seven months after infection and a fifth had not been able to return to previous levels of work for six months. Other studies have found that patients can have enduring neurological problems that affect their memory, attention and sense of smell six months after infection with Covid-19. Of course, we will need to gather more data to find out just how representative these problems are among those with the condition.
Research into Long Covid is still in its infancy though – we still have no clear idea of just how long the condition will last. Covid-19 has simply not yet been around for long enough.
A related coronavirus that caused the far smaller SARS outbreaks between 2002-2004 showed signs of causing similar long term problems that left some people unable to work for up to 36 months after infection. Another study found that 40% of those who recovered from SARS still suffered chronic fatigue four years later. We know that SARS tended to cause severe disease far more often than Covid-19 does. But there also does not seem to be any correlation between the seriousness of Covid-19 and the long-term illness.
What is clear is that with more than 100 million Covid-19 cases worldwide, the health burden left by Long Covid could be enormous. In the UK alone, there could be hundreds of thousands of patients who endure symptoms for many months, putting further pressure on an already stretched healthcare service. This will not only impact the lives of those who are suffering, but also has the potential to create an ongoing economic burden if they find themselves unable to work.
But amid the stories of those suffering from Long Covid there are also glimmers of hope. At the start of 2021, Paul Garner reported that his health had finally returned. With the right support, and the help of the scientific community, hopefully many others can follow him.