Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Extracellular vesicles and the tumour microenvironment
Scientific discussion meeting organised by Dr Daniel Lambert, Dr Dave Carter, Dr Stuart Hunt, Dr Aled Clayton and Dr Andrew Devitt.
This meeting will explore the fundamental roles that extracellular vesicles can play in cell-to-cell communication, with a specific focus on their role in the tumour microenvironment. The importance of these two areas has emerged in the past decade and this meeting will explore the synergies that exist between the two fields.
The schedule of talks and speaker biographies are available below. Speaker abstracts will be available closer to the meeting date. Recorded audio of the presentations will be available on this page after the meeting has taken place.
Meeting papers have now been published in Philosophical Transactions B.
Enquiries: Contact the Scientific Programmes team
Organisers
Schedule
Chair

Dr Dan Lambert, University of Sheffield

Dr Dan Lambert, University of Sheffield
Dan Lambert completed his undergraduate degree and PhD at the University of Liverpool before moving to carry out post-doctoral research at the University of Leeds in Prof. Anthony Turner’s lab. Here he studied the mechanisms regulating a membrane proteinase recently discovered in the lab, angiotensin-converting enzyme-2 (ACE2), an enzyme involved in blood pressure regulation and the receptor for the SARS coronavirus. He discovered a proteinase, ADAM17, was responsible for cleaving ACE2 from the cell surface and releasing a functionally active ectodomain. This led Dan to examine mechanisms of proteolysis of membrane proteins more broadly, and latterly the role of non-coding RNA in regulating membrane proteolysis and cell:cell communication. In 2008 he set up his own lab at the University of Sheffield which examines how non-coding RNA, membrane bound proteases and extracellular vesicles influence cellular interactions in the tumour microenvironment and in in fection.
| 09:05 - 09:30 |
Tumour extracellular vesicles and breast cancer metastasis
In spite of significant improvements in treatments and survival rates, metastatic breast cancer remains one of the leading causes of cancer-related deaths in women worldwide. Taxanes are microtubule-stabilizing agents largely employed as cytotoxic agents for breast cancer treatment, both in the adjuvant and neoadjuvant setting. Increasing evidence suggests that the cancer cells of primary tumors release extracellular vesicles (tEVs), which can facilitate the homing of metastatic cells to target organs. We found that paclitaxel – a lead taxane – enhances tEV release from murine breast cancer cells, both in vitro and in vivo. I will present the functional implications of this phenomenon in the context of breast cancer. Furthermore, I will discuss the determinants of microRNA sorting to EVs, and the significance of EV-mediated microRNA transfer to acceptor cells. 
Dr Miki De Palma, École Polytechnique Eédérale de Lausanne

Dr Miki De Palma, École Polytechnique Eédérale de LausanneMiki obtained his Ph.D. in 2004 from the University of Turin Medical School, Italy, where he studied the contribution of bone marrow-derived cells to tumor angiogenesis under the direction of gene therapy pioneer Luigi Naldini. He performed post-doctoral training at the Telethon Institute for Gene Therapy (TIGET) in Milan, to develop gene transfer strategies for reprogramming tumor-infiltrating monocytes into anti-tumoral immune cells. In 2011, he was appointed tenure-track assistant professor at the ISREC institute of the Swiss Federal Institute of Technology of Lausanne (EPFL), Switzerland, where he teaches cancer biology and leads a group of enthusiastic young scientists. By employing genetic models of cancer and cell-engineering strategies based on lentiviral gene transfer, the De Palma’s lab investigates the interplay among macrophages, blood vessels and T cells in tumors, primarily by focusing on angiogenic signaling, immune checkpoints, microRNA regulation, and secreted exosomes. Miki received a European Research Council grant and a number of prizes from scientific societies. He has co-organized, and is routinely invited to, international conferences on angiogenesis, tumor immunology and cancer research, and serves on the advisory boards of several scientific journals, including Science Translational Medicine (AAAS), Cell Reports (Cell press), and Cancer Immunology Research (AACR). In his spare time, he enjoys travelling to sub-saharan Africa and writing articles and books on the taxonomy of the African fruit and flower beetles. |
|
|---|---|---|
| 09:30 - 09:45 | Discussion | |
| 09:45 - 10:15 |
An apoptosis-driven 'onco-regenerative niche': roles of tumour-associated macrophages and extracellular vesicles
Apoptosis is a well-established anti-oncogenic cell-death programme. Paradoxically, high apoptosis indices in tumours are closely coupled with poor prognosis. Indeed, where it has been studied, cell loss is a striking feature of high-grade cancers, illustrating the importance of considering malignant disease as an imbalance between cell gain and cell loss rather than as a unidirectional disorder of cell gain alone. In addition to orchestrating cell loss, apoptosis can signal regenerative responses; for example compensatory proliferation in other cells. Accumulating evidence suggests that normal tissue repair and regenerative processes are hijacked in the malignant tissue microenvironment such that cancer may be likened to a “wound that fails to stop repairing”. We have proposed that a critical requirement for the successful growth, progression and re-growth of malignant tumours is a complex niche, conceptually termed the “onco-regenerative niche”, which is composed, in addition to transformed neoplastic cells, of normal cells and factors activated as if in tissue repair and regeneration. Our work is based around the hypothesis that tumour cell apoptosis, macrophage activation and endothelial activation are key, interlinked elements of the onco-regenerative niche and that apoptotic tumour cell-derived extracellular vesicles (Apo-EVs) provide critical intercellular communication vehicles of the niche. In aggressive B-cell lymphoma, tumour cell apoptosis promotes both angiogenesis and the accumulation of pro-tumour macrophages in the lymphoma microenvironment. Furthermore, lymphoma-derived apo-EVs have potent pro-tumour potential. These findings have important implications for the roles of apoptosis in regulation of malignant diseases and for the efficacy of apoptosis-inducing anti-cancer therapies. 
Professor Christopher D Gregory, MRC Centre for Inflammation Research

Professor Christopher D Gregory, MRC Centre for Inflammation ResearchProfessor Chris Gregory holds the Chair of Inflammatory Cell Biology at the University of Edinburgh College of Medicine and Veterinary Medicine and is Deputy Director of the University of Edinburgh/MRC Centre for Inflammation Research. He leads the Inflammation and Cancer Group in the Centre and has a research track record spanning three decades in the field of apoptosis and especially apoptotic cell clearance. He has particular interests in the regulation of apoptosis in tumours, especially non-Hodgkin lymphomas, the mechanisms underlying the interaction of apoptotic tumour cells with innate immune cells including tumour-associated macrophages, the consequences of such interactions for anti-tumour immunity and the manipulation of these mechanisms for therapeutic gain. Current research is focused on how extracellular vesicles produced by apoptotic tumour cells promote tumour progression and relapse. Core support for current research activities is provided mainly from Bloodwise (formerly Leukaemia and Lymphoma Research) and from the MRC. |
|
| 10:15 - 10:30 | Discussion | |
| 11:00 - 11:15 |
Cellular stress sensors mTORC1 switches exosome biogenesis and secretion pathways to influence the tumour microenvironment
Contributory talk given by Associate Professor Deborah Goberdhan. Cancer cells can adapt to nutrient starvation and growth inhibitory drugs by communicating with their neighbours via secreted soluble factors, exosomes and other extracellular vesicles. Exosomes are commonly believed to originate in late endosomal multivesicular bodies, but the intracellular mechanisms modulating their functions remain poorly characterised. Here a new type of exosome biogenesis pathway involving Rab11-positive recycling endosomes is identified that releases exosomes with enhanced reprogramming activities. This pathway is present in both human cancer cells and an in vivo Drosophila model of exosome secretion. Using the fly model the biogenesis of these different exosome subtypes can be visualised in living tissue for the first time. Inhibiting the glutamine-sensing PAT4 amino acid transporter blocks a specific form of mTORC1 signalling, leading to the preferential release of exosomes from recycling endosomes. Functionally, these stress-induced exosomes orchestrate signalling in recipient cells, which promotes pro-tumorigenic microenvironmental changes and cancer growth. Therefore in cancer cells the mTORC1 signalling hub senses microenvironmental stresses and then modulates exosome secretory pathways to drive tumour adaptation. These findings may partly explain why mTORC1 inhibitors often have poor clinical efficacy, and highlight the importance of distinguishing exosomal sub-types when defining their effects on the tumour microenvironment. |
|
| 11:15 - 11:30 |
Tetherin exosomes
Contributory talk given by James Edgar Edgar et al demonstrate that exosome release can be induced in HeLa cells upon inhibition of the V-ATPase, and that exosomes are observed in clusters at the plasma membrane. Such clustering shows striking similarities to clusters of retroviruses, which are attached to the plasma membrane by tetherin. To determine whether tetherin also attaches exosomes, it was knocked out and this resulted in a 4-fold reduction in plasma membrane-associated exosomes, with a concomitant increase in exosomes discharged into the medium. Such phenotype could be rescued by expression of wild-type tetherin but not tetherin lacking its GPI anchor. Edgar et al propose that tetherin may play a key role in exosome fate, determining whether they participate in long-range or short-range interactions. |
|
| 11:30 - 11:45 | Discussion | |
| 11:45 - 12:15 |
Can glioblastoma extracellular vesicles drive normal astrocytes towards a tumour-enhancing phenotype?
Glioblastomas (GBMs, WHO grade IV astrocytomas) are the worst of the central nervous system tumors; despite maximum (and damaging) therapeutic intervention, median survival time for patients is <15 months, and overall quality of life is poor. These abysmal outcomes have changed little in 20 years. Clearly, our current therapies are inadequate; we need innovative strides in understanding GBM biology to rectify this situation. One “hot” research area is that of the impact of tumor extracellular vesicles (EVs) on normal recipient cells. Tumor EVs have extraordinary abilities to manipulate tumor microenvironments and recipient cells both proximally and distally. Tumor EVs prepare the “metastatic niche” for circulating tumor cells prior to colonization of a target organ, deflect immune responses, and alter normal cells. Thus, tumor EVs impact recipient cells to support tumor growth and progression, which undoubtedly holds true for GBMs as well. However, little is known about effects of GBM EVs on normal astrocytes—do GBM EVs drive astrocyte phenotypic changes, potentially making the astrocytes into tumor promotors? The answers could re-shape our paradigms on gliomagenesis, particularly for recurrent tumors. Here we show that GBM EVs activate cancer-type signaling pathways in recipient astrocytes, promoting astrocyte migration towards the EVs, as well as astrocyte anchorage-independent growth in soft agar. Astrocytes release of various factors to generate a tumor-promoting milieu with increased tumor cell growth. We discuss the consequences of these phenomena in the context of our current therapies with a view towards therapeutic improvement. 
Dr Michael Graner, University of Colorado Denver

Dr Michael Graner, University of Colorado DenverGraner is an Associate Professor of Neurosurgery, but he is not even remotely a neurosurgeon, and cannot fix your back. He is a recovering biochemist pretending to be an immunologist. He somehow obtained a PhD from the University of Illinois, post-doc’d and became fake faculty at the University of Arizona (where he moved from working on fruit flies to Pediatric Oncology, a perfectly logical move), and then joined the Tisch Brain Tumor Center at Duke University. There, he became enamored with the bizarre fat balls known as exosomes. Having lost all tolerance for biting insects and absurd humidity, he moved to the University of Colorado Denver, at the Anschutz Medical Campus, which is actually in Aurora, where he continues to study exosomes, stress responses, and cancer immunology. |
|
| 12:15 - 12:30 | Discussion |
Chair

Dr Andrew Devitt, Aston University

Dr Andrew Devitt, Aston University
Current research within the my group at Aston University is focused upon the structure-function analyses of apoptotic cell-derived extracellular vesicles (EV). This stems from my long-term interest in the role of the innate immune system in mediating removal of apoptotic cells. My group has demonstrated that EV can exert profound effects on the immune system by acting as potent promoters of phagocyte recruitment. This is relevant to the study of the tumour microenvironment as the interaction between dying tumour cells and recruited leukocytes has been shown to impact tumour development.
| 13:30 - 14:00 |
Kesley Attridge
|
|
|---|---|---|
| 14:00 - 14:15 | Discussion | |
| 14:15 - 14:45 |
Biochemical characterisation and immune effects of different subtypes of extracellula vesicles released by dendritic cells
Cells secrete into their environment different types of extracellular vesicles (EVs) that have distinct structural and biochemical properties depending on their intracellular site of origin. Exosomes are a subtype of EVs with a mean diameter lower than 150 nm that are formed inside multivesicular compartments of the endocytic pathway. Exosomes secreted by dendritic cells (DCs) have been shown to bear functional MHC class I and class II molecules able to activate cognate T cells. These findings motivated the use of DC-derived exosomes in cancer clinical trials, although with limited clinical effects. Other EVs also bear functional immune molecules and may thus represent alternative immunotherapy tools. However, side-by-side comparison of the immune effects of exosomes and other EVs has never been comprehensively performed. Here, we have isolated different subtypes of EVs simultaneously released by live human primary DCs and extensively characterize their proteome as well as their effects on primary lymphocytes. Subtypes of EVs included large ones (> 200nm diameter) budding from the plasma membrane of live cells, small ones (< 150 nm diameter), which include exosomes and other non-exosomal sEVs, and intermediate-size EVs, which we separated by a combination of differential ultracentrifugation, floatation into density gradients and immuno-isolation via different tetraspanins. Comparative proteomic analysis of these different EVs allowed us to propose a new cartography of EV-associated protein markers, including combinations that define endosome-derived exosomes. Functionnally, we show that all these EVs efficiently induced T lymphocyte proliferation, but that they differently skew the CD4 T helper immune response. Our results provide a refined framework for the use of EVs in immunotherapy. 
Dr Clothilde Thery

Dr Clothilde TheryClotilde Théry, PhD, is PI of a team entitled « Exosomes and tumor growth » at Institut Curie, Paris, France, in the “Immunity and Cancer” INSERM department. She is an internationally recognized expert of EVs in general, and exosomes in particular, owing to 15 years expertise in the domain. Since 2007, her team has focused on unraveling the in vivo physiological or pathological functions of these vesicles, by continuously going from cell biology approaches of their modes of formation to application of this knowledge to in vivo situations. She is regularly invited to write reviews on the subject of exosomes, EVs, their immune functions and their biogenesis (Nature Rev Immunol 2009; Traffic 2011; Curr Op Cell Biol 2014, Annual Rev Cell Biol 2014, Cell 2016), and has published since 1999 several articles on the subject (e.g. J Cell Biol 1999, Nature Immunol 2002, Blood 2005, Nature Cell Biol 2010, Cancer Res 2012, PNAS 2016). C. Théry has been Secretary General of the International Society for Extracellular Vesicles (ISEV) from 2012 until 2016, and is co-editor in chief of the Journal of Extracellular Vesicles, since its creation in 2012. |
|
| 14:45 - 15:00 | Discussion | |
| 15:30 - 16:00 |
Is there more to the secretory phenotype in senescent cells?
Cellular senescence is an important tumour suppressive mechanism to prevent the propagation of damaged cells. It induces a permanent cell cycle arrest, where the cells are metabolically and transcriptionally active. Senescent cells undergo extensive changes in gene expression, including the expression of cell cycle inhibitors and a distinctive secretory phenotype called the SASP (senescence-associated secretory phenotype), which influences the tissue microenvironment. Senescent cells accumulate in preneoplastic lesions; however, the mechanisms regulating senescence and how senescent cells alter their surrounding microenvironment is not well known. In fact, conflicting data suggests that the SASP has both anti-oncogenic and pro-oncogenic properties depending on the tissue and on the context. Here, we will explore a potential role for extracellular vesicles (EV) secreted by senescent cells in contributing to this biphasic role for the SASP during senescence activation. Our data would help identify appropriate therapeutic targets and biomarkers to tackle senescent cells and cancer at the very early stages of the disease. 
Dr Ana O'Loghlen, Queen Mary, University of London

Dr Ana O'Loghlen, Queen Mary, University of LondonAna O'Loghlen obtained her PhD from the Complutense University of Madrid in 2005 studying the role for oxidative stress during brain ischemia. After a short postdoc at the CNIO with Angel Nebreda, she joined Jesus Gil’s lab to study novel regulatory pathways controlling cellular senescence. In 2013 she started her own lab in Queen Mary University in London where she continues to study uncharacterized mechanisms regulating senescence. |
|
| 16:00 - 16:15 | Discussion | |
| 16:15 - 16:45 |
Vesicular communication in cancer
Our studies elucidate the role of vesicular communication in tumor development, and how vesicular transport mechanisms can be exploited for specific targeting of treatment resistant cells of the hypoxic tumor microenvironment. Extracellular vesicles (EVs) represent relatively new signaling organelles in cell-cell communication that can carry complex biological information and elicit a pleiotropic response in recipient cells. We have found that EVs play an important role during hypoxia-mediated tumor development, and that EVs may provide a novel source of non-invasive biomarkers of the hypoxic tumor stress response. Further studies identified a key role of heparan sulfate proteoglycan-mediated endocytosis for the uptake and functional effect of EVs. More recently, we found that hypoxia down-regulates constitutive endocytosis through caveolin-1-mediated inhibition of dynamin-dependent, membrane raft endocytosis. However, several proteins can override caveolin-1 negative regulation, exhibiting increased internalization at hypoxia, further allowing antibody-mediated cytotoxin delivery and killing specifically of hypoxic cells. These data indicate that caveolin-1 modulates cell-surface proteome turnover at hypoxia with potential implications for specific targeting of the hypoxic tumor microenvironment. Based on these findings we will further explore the hypothesis that transport vesicles promote tumor aggressiveness and constitute novel therapeutic targets specifically related to typical features of the tumor microenvironment. 
Dr Matthias Belting, Skåne University Hospital

Dr Matthias Belting, Skåne University HospitalMattias Belting is professor of Clinical Oncology and senior consultant of Neuro Oncology at Lund University, Lund, Sweden. He received his PhD in medicinal chemistry in 1999, followed by postdoc visits in tumor biology at UCSD & The Scripps Research Institute, La Jolla. Belting currently heads The Tumor Microenvironment group that gathers clinicians and experimental researchers with the aim to elucidate how stress-related phenomena, such as hypoxia and coagulation activation, drive tumor development and the role extracellular vesicles as mediators and biomarkers of these events. |
|
| 16:45 - 17:00 | Discussion |
Chair

Dr Stuart Hunt, University of Sheffield

Dr Stuart Hunt, University of Sheffield
Dr Stuart Hunt completed his undergraduate degree in Biomedical Science (BSc) at The University of Sheffield. He then pursued his interest in molecular biology at The University of Manchester, whilst studying for his Master’s degree. He then returned to The University of Sheffield to study for his PhD in the Department of Molecular Biology and Biotechnology. After a period of post-doctoral research, he was appointed as a lecturer in The School of Clinical Dentistry. Stuart has established a research group that focuses on the role of extracellular vesicles (EV) in head and neck cancer. His current research projects specifically address the differences in molecular cargo of EVs derived from HPV+ and HPV- oropharyngeal tumours, the use of EVs to predict the stage of oral cancer, and the potential use of salivary EVs for the early diagnosis of oral cancer.
| 09:00 - 09:30 |
The role of EVs in NK cell-dependent immuunosurveillance of cancer
Extracellular vesicles (EVs) are important mediators of intercellular communication and act on the adjacent stroma as well as in the periphery. Recently, EVs have been recognized to play a pathophysiological role in various diseases such as cancer. Tumor cell-derived exosomes (Tex) have been shown to educate non-malignant cells to provide a tumor supporting microenvironment, which helps to circumvent immune detection and elimination. We identified a disease-related mRNA signature in vesicles from malignant B cells (Chronic Lymphocytic leukemia, CLL), which was even pronounced upon toll like receptor engagement used as a milieu-mimics. The transfer of such mRNAs to healthy bystander cells was detectable indicating that CLL-released vesicles spread tumor-milieu instructions within the CLL microenvironment. However, Tex with anti-tumor, immune-activating properties were described as well, which reflects the complexity of EVs. Activation of the innate immune receptor retinoic acid-inducible gene I (RIG-I) triggered the secretion of EVs from tumor cells, which exert anti-tumor activity in vitro and in vivo. RIG-I-induced EVs exhibited an increased expression of the NKp30-ligand (BAG6, BAT3) on their surface, triggering NK cell-mediated lysis of tumor cells via activation of the cytotoxicity NK cell-receptor NKp30. Moreover, systemic administration of RIG-I-induced tumor-EVs showed a potent anti-tumor activity in a melanoma mouse model in vivo. In conclusion our data establish a new RIG-I and EV-dependent pathway leading to NK cell-mediated tumor cell killing. The role of EVs as messengers affecting NK cell function in health and disease will be discussed. 
Professor Elke Pogge von Strandmann, University of Cologne

Professor Elke Pogge von Strandmann, University of CologneElke Pogge von Strandmann graduated 1995 as a PhD from the University of Essen, Institute for Cell Biology and Tumor Research. Until 2002 she was a postdoctoral fellow and later a group leader at this Institute. Since 2002 she is heading the Innate Immunity Group at the University Clinic Cologne. Her research aims to elucidate the molecular cross-talk of immune/bystander cells with tumor cells within the tumor microenvironment on the molecular level. Her work contributed to a better basic understanding of immune evasion from NK cell-based immune surveillance in Hodgkin lymphoma and Chronic Lymphocytic Lymphoma. Based on this, the group proceeds to develop novel innovative therapeutic strategies to fight tumors using recombinant ligands for activating NK cell-receptors. |
|
|---|---|---|
| 09:30 - 09:45 | Discussion | |
| 09:45 - 10:15 |
Analysing the effects of extracellular vesicles on cancer invasion using human myoma tissue derived extracellular matrixes
Translational cancer research has lacked human tissue in vitro models that mimic the natural tumor microenvironment matrix (TMEM). The 3D invasion pattern has been studied with organotypic models composed of rat tail type I collagen combined with mouse tumor derivatives, such as Matrigel®. However, these classical methods that mix matrixes from different species do not accurately mimic the composition of human TME. Our group has developed a 3D invasion assay using human uterine leiomyoma tissue discs. These hypoxic discs contain all essential TME components for in vitro invasion experiments. Both in native and lyophilized forms, these discs promote invasion and growth of the cancer cells - unlike e.g. healthy heart tissue. The invasion efficiency in the myoma discs can be analyzed by determining the degradation of collagen fibers together with histological and immunohistological staining of the tissue sections. Proteome analysis of myoma rinsing media revealed migration-enhancing factors whereas fragments derived from heart tissue rinsing media inhibited cancer migration. Myoma discs fit also for co-culture experiments of various TME cells, such as carcinoma associated fibroblasts, macrophages and inflammatory cells. We have also prepared myogel product from leiomyoma according to the method described for the preparation of Matrigel®. Myogel provides an excellent method for analyzing cancer cell migratory, invasive or adhesive properties, as well as potential chemotherapeutic compounds. Recently, myoma matrixes are used to test the effects of extracellular vesicles for cancer invasion. Thus, myoma discs together with myogel offer a practical human “TMEM mimicking kit” for translational cancer research purposes. 
Professor Tuula Salo, University of Oulu

Professor Tuula Salo, University of OuluTuula Salo, DDS, PhD, specialist in oral pathology, is a part-time professor of oral pathology, at the Dept of Oral and Maxillofacial Diseases, University of Helsinki and at the Cancer and Translational Research Unit, University of Oulu, Finland. She is a visiting professor in Piracicaba Dental School, Sao Paulo Campinas, State University, Brazil. As a senior Physician in Oral Pathology she works at Oulu and Helsinki University Hospitals. Professor Salo´s research has recently focused mainly on the analyses of factors in tumor microenvironment effecting on oral cancer progression and invasion. She has developed 3D in vitro human tumor tissue derived models, myoma discs and myogel, for cancer invasion assays. Salo has published over 270 original articles in refereed journals which have been cited over 10 000 times and her HI is 62. |
|
| 10:15 - 10:30 | Discussion | |
| 11:00 - 11:15 |
Cancer exosomes establish a prometastatic inflammatory loop by engaging mesencgymal stem cells
Contributory talk given by D. Michiel Pegtel Metastasis formation and resistance to therapy, for example via STAT3 activation in tumor cells, could be a consequence of driver-mutations in cancerous ‘stem’ cells or of cancer-stroma interactions, but a role for mesenchymal stem stem cells (MSCs) is poorly understood. This talk will discuss how we explored in an in vivo osteosarcoma (OS) model how tumor exosomes may engage MSCs to facilitate tumor progression. |
|
| 11:15 - 11:30 |
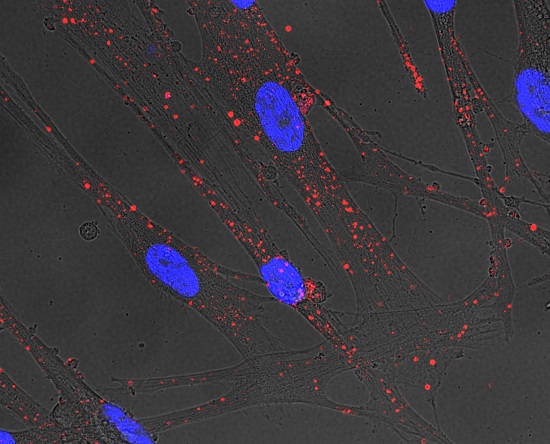
Extracellular vesicles and the pre-metastatic niche: a deadly conversation between prostate tumours and the bone
Contributory talk given by Victoria James
The popular ‘seed and soil’ hypothesis proposes that organ preference patterns of metastasis result from favourable interactions between the metastatic cancer cells (‘seed’) and the organ microenvironment (‘soil’). However, what is less clear is whether primary tumours communicate with secondary sites in advance of tumour cell arrival, to create a ‘pre-metastatic niche’, to enhance tumour-cell colonisation at the most inefficient stage of metastasis. The role of extracellular-vesicles in this communication process remains to be explored. In order to investigate how the cargo of prostate cancer (PCa) EVs could act to reprogramme the cells of the bone, to potentially create a supportive pre-metastatic niche. We have adapted a novel RNA tracking technique, to trace the route of the RNA cargo from PCa cells via EVs into recipient bone cells (osteoblasts), identifying several osteoblast specific RNAs suggesting PCa cells may selectively target cells of the bone with EV-mediated communication. Exposure of osteoblasts to PCa-EVs results in phenotypic changes indicative of microenvironment remodelling. Moreover, our data indicates treatment of the extracellular-environment can effectively block the uptake of PCa-EVs resulting in a reversal of the EV-activated osteoblast phenotype. |
|
| 11:30 - 11:45 | Discussion | |
| 11:45 - 12:15 |

Dr Stuart Hunt, University of Sheffield

Dr Stuart Hunt, University of SheffieldDr Stuart Hunt completed his undergraduate degree in Biomedical Science (BSc) at The University of Sheffield. He then pursued his interest in molecular biology at The University of Manchester, whilst studying for his Master’s degree. He then returned to The University of Sheffield to study for his PhD in the Department of Molecular Biology and Biotechnology. After a period of post-doctoral research, he was appointed as a lecturer in The School of Clinical Dentistry. Stuart has established a research group that focuses on the role of extracellular vesicles (EV) in head and neck cancer. His current research projects specifically address the differences in molecular cargo of EVs derived from HPV+ and HPV- oropharyngeal tumours, the use of EVs to predict the stage of oral cancer, and the potential use of salivary EVs for the early diagnosis of oral cancer. |
|
| 12:15 - 12:30 | Discussion |
Chair

Dr Ryan Pink

Dr Ryan Pink
After completing a Molecular biology PhD on Dietary linked Oesophageal cancer in developing world South Africa, he worked around Europe on point-of-care early diagnostic cancer tools. Ryan is now a Lecturer in Molecular Biology and Genomics at Oxford Brookes University focusing on the effect of extracellular vesicles on muscle and neuron development on Earth and in space. His lab focuses on gene expression, characterisation and function (Microarray, RNAseq, Nanopore). Ryan teaches Medical Genomics and develops medical research projects across NHS, Oxford Brookes University and University of Oxford for the Oxford Academic Health Science Centre. He is widely involved in Public Engagement projects from Art to science festivals and has presented and published his work internationally, including House of Commons, London Science Museum, Natural History Museum.
| 13:30 - 14:00 |
Role of extracellular vesicle-mediated angiogenesis in hematologic neoplasias
It is widely accepted that tumor cells can affect surrounding cells by changing the tumor microenvironment (TME) from a normal to a tumor-supportive state that promotes tumor cell growth and survival, invasion, and chemoresistance. Like the TME in solid tumors, a tumor-supportive bone marrow microenvironment is required for disease progression in hematologic neoplasia. Bone marrow is a highly vascular tissue that is already hypoxic in nature. Increased bone marrow angiogenesis is related to disease severity and progression. Extracellular vesicles, especially exosomes, are currently recognized as mediators of intercellular communication. Hypoxia is a major regulator of exosomal content and affects angiogenesis in various types of hematologic neoplasia. For instance, exosomes secreted by multiple myeloma cells with chronic hypoxia enhance angiogenesis by targeting factor-inhibiting hypoxia-inducible factor-1 via miR-135b. We will discuss the exosome-mediated cell–cell interactions that modulate tumor angiogenesis, and a possible role of hypoxia in hemtologic neoplasias. 
Junko H. Ohyashiki, Tokyo Medical University

Junko H. Ohyashiki, Tokyo Medical UniversityJunko studied her M.D. at Tokyo Medical University in 1972-1978, followed by her Ph.D at TokyoMedical University, Tokyo Japan. In 1984-1986 she was a Research fellow at the Department of Genetics and Endocrinology, Roswell Park Memorial Institute, Buffalo, NY, USA. In 1987-2003 she was an Assistant professor at Department of Hematology, Tokyo Medical University. In 2003-2008 she was an Associate professor at Intractable Disease Research Center, Tokyo Medical University. Since 2009 she has been a professor at the Department of Molecular Oncology, Institute of Medical Science, Tokyo Medical University. She has a variety of awards including Medical Award of The Tokyo Medical Association, Award of Japan Medical Woman’s Association, and Research Grant, Foundation for promotion of Cancer Research. Her interests lie in non-coding RNA in cancer and the role of telomeres and telomerase in cancer and aging. |
|
|---|---|---|
| 14:00 - 14:15 | Discussion | |
| 14:15 - 14:45 |
Defining the role of tumour-secreted exosomes in metastasis
Cancer is a systemic disease, while most of the research effort has been focused on analyzing the primary tumor, there is a lack of information on how the tumor microenvironment influences metastasis. The importance of the microenvironment in metastasis is now fully acknowledged. Prominent roles for stromal cells, such as fibroblasts, endothelial cells, lymphatic endothelial cells, bone marrow-derived cells, soluble factors and secreted vesicles have been established. Our studies in metastatic melanoma demonstrated that tumor exosomes are a major tumor-derived factor that acts systemically to promote bone marrow-derived cells (BMDCs) recruitment to the tumor and metastatic microenvironments. We have demonstrated the role of tumor-secreted exosomes in premetastatic niche formation and metastatic organotropism. We are currently analyzing the dynamics of tumor-derived exosomes in the lymphatic system and their role establishing the pre-metastatic niche formation within the lymph node microenvironment. We found that tumor-secreted exosomes inducing a prolymph(angio)genic program and reprogramming of lymphatic endotelial cells within pre-metastatic lymph nodes. Our data support that tumor-secreted exosomes can be considered as a novel biomarker of lymph node metastasis. We found a signature associated to melanoma lymph node metastasis and we are currently analyzing circulating exosomes in the lymphatic fluid of cancer patients as a new approach to define new markers involved in tumor metastasis. Our data suggest that tumorsecreted exosomes act locally and systemically remodeling the lymphatic system favoring metastasis. 
Dr Hector Peinado, Spanish National Cancer

Dr Hector Peinado, Spanish National CancerDr Peinado did his PhD in the laboratory of Dr. Amparo Cano in Madrid (Spain, Biomedical Research Institute “Alberto Sols”) where he specialized in analyzing Epithelial to Mesenchymal Transition Mechanisms. In this lab they described the molecular mechanisms of EMT regulated by Snail transcription factor and Lysyl Oxidase 2 (EMBO J (2005) 24:3446-58, Nat. Rev Cancer. (2007). 7:415-28). He defined a role for beta-catenin in regulating cancer stem cell behavior in skin cancer (Nature. (2008) 452:650-3). Hector then joined Dr. Lyden’s laboratory as a postdoctoral associate in 2008 to study the crosstalk between tumor cells and bone marrow derived cells during metastatic progression. During these years Hector developed his career as an independent researcher with an excellent collaboration with Dr. Lyden. In 2010, was appointed to a Faculty Position in the Department of Pediatrics at WCMC and in 2013 he was promoted to Assistant Professor. Hector’s work has recently defined that tumor-secreted exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype (Nature Medicine. 2012. (18): 883-891.). In 2015, he joined the CNIO as Group Leader of the Microenvironment and Metastasis laboratory with a Ramon y Cajal contract. His current research goals are focused on understanding the crosstalk between the tumor and its microenvironment by secreted factors during lymph node metastasis and determine new targets to block metastasis. |
|
| 14:45 - 15:00 | Discussion | |
| 15:30 - 16:00 |
Extracellular vesicles in the tumour microenvionment
MicroRNAs (miRNAs) are small non-coding RNAs (ncRNAs) that epigenetically regulate gene expression by affecting their translation at a post-transcriptional level. It has been shown that miRNAs can be functionally shuttled among neighboring cells, as cargo of extracellular vesicles. The traditional mechanism of action of miRNAs implies that these small ncRNAs act by binding mostly (but not exclusively) to the 3’-untranslated region of target messenger RNAs, therefore impairing their translation into proteins. Such a dogma has been recently challenged by our discovery that miRNAs in extracellular vesicles can actually also work as “hormones” by binding to Toll-like receptor 8 (TLR8) in surrounding Tumor-Associated Macrophages (TAMs), within the Tumor Microenvironment. The binding of miRNAs to a receptor (that we called, miRceptor) leads to the activation of the NF-kB signaling and to an increased TAM secretion of cytokines with a pro-inflammatory and pro-tumoral role. Moreover, we showed that the miRNA-miRceptor interaction leads to the secretion of TAM-derived extracellular vesicles containing miRNAs that are shuttled back to cancer cells, where they target genes responsible for an increased resistance to chemotherapy. This aberrant cross-talk between cancer cells and TAMs, mediated by miRNAs in extracellular vesicles, can be exploited for the design and testing of new anti-cancer therapy, and to prevent/overcome the development of resistance to chemotherapy. 
Dr Muller Fabbri, University of Southern California

Dr Muller Fabbri, University of Southern CaliforniaDr. Muller Fabbri is Assistant Professor of Pediatrics and Molecular Microbiology and Immunology at Children’s Hospital Los Angeles (CHLA), Keck School of Medicine of the University of Southern California. Dr. Fabbri has provided the first evidence of the existence of epi-miRNAs, and has described a complex miRNA-based network responsible for the prognostic significance of chromosomal aberrations in chronic lymphocytic leukemia. More recently, Dr. Fabbri has identified a completely new mechanism of action for miRNAs as ligands of Toll-like receptors. Dr. Fabbri is author of more than 60 peer reviewed publications, he has authored several book chapters, serves in the Editorial Board of 6 international scientific Journals. Dr. Fabbri’s lab at CHLA is focused on studying how microRNAs (and other non-coding RNAs) are communicating between cancer cells and surrounding cells of the tumor microenvironment and how this affects cancer biology and the development of resistance to chemo and radiotherapy. |
|
| 16:00 - 16:15 | Discussion | |
| 16:15 - 17:00 | Panel discussion: future directions |