Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Meeting the challenges of modelling neurodegenerative disease in mice
Theo Murphy international scientific meeting organised by Professor Elizabeth Fisher, Professor Giampietro Schiavo and Dr Pietro Fratta
New technologies for engineering the mouse genome are increasingly sophisticated. However, mouse models of neurodegeneration try to recapitulate human late-onset disorders in an animal that lives for two years and has important differences in physiology and biochemistry. How can we best model neurodegeneration? What features matter? What has given us most insight? What is the future we would like?
The schedule of talks and speaker biographies will shortly be available below. A draft programme is available to download.
Recorded audio of the presentations will be available on this page after the meeting has taken place.
Attending this event
- Free to attend
- Advanced registration essential (please request an invite)
- Catering and accommodation available to purchase during registration
Enquires: Contact the Scientific Programmes team
Organisers
Schedule
Chair

Professor Giampietro Schiavo, UCL Institue of Neurology, UK

Professor Giampietro Schiavo, UCL Institue of Neurology, UK
Professor Giampietro Schiavo obtained his PhD from the University of Padua, Italy, and received postdoctoral training at the Department of Biomedical Studies, University of Padua, Italy, and at the Memorial Sloan Kettering Cancer Center in New York, USA, under the supervision of Professors Cesare Montecucco and James Rothman, respectively. He was then recruited as junior group leader at the Cancer Research UK London Research Institute (then Imperial Cancer Research Fund), where he led the Molecular NeuroPathobiology Laboratory until 2013. He then moved to the Institute of Neurology at University College London as a full Professor in 2014. The goal of Professor Schiavo’s research is to understand the mechanisms underlying axonal retrograde transport how neurons control the uptake and sorting of ligands in health and disease conditions.
| 09:10 - 09:30 |
Genomic humanisation and other technologies in mouse

Professor Allan Bradley FRS, The Wellcome Trust Sanger Institute, UK

Professor Allan Bradley FRS, The Wellcome Trust Sanger Institute, UK |
|
|---|---|---|
| 09:30 - 09:40 | Discussion | |
| 09:40 - 10:00 |
An expanding role for rAAV in complex neurodegenerative mouse modelling
Neurodegenerative diseases are typically complex; involving both genetic and environmental (including age) factors. This complexity presents a major challenge to the mouse disease-modelling community. Recombinant adeno-associated virus (rAAV) was first discovered in 1965 as a contaminant of simian adenovirus preparations. Since that time, rAAV has been evolved by researchers into a critical tool for transgenesis, applicable to: mouse modelling, mechanistic analyses, and gene therapy. Most recently, three factors have further expanded the applicability of rAAV: 1) relaxation of biohazard regulations enabling the use of rAAV in vitro and in vivo in most research laboratories; 2) isolation, directed evolution, and rationale design of new capsid (protein viral shell) variants that confer novel transduction capabilities to the virus; and 3) implementation of gene regulation by the development of MiniPromoters small enough to fit into the rAAV genome, but still able to provide cell-type restricted expression. For example, a virus that can efficiently cross the blood brain barrier, widely transduce the brain, but only express the transgene in a subset of serotonergic dorsal raphe neurons. With these new viral tools, scientists are combining genetic predisposition with rAAV transgenesis to address question underlying the mechanisms of neurodegeneration, and generate new more complex mouse models. 
Professor Elizabeth M. Simpson, Centre for Molecular Medicine and Therapeutics (CMMT), University of British Columbia, Canada

Professor Elizabeth M. Simpson, Centre for Molecular Medicine and Therapeutics (CMMT), University of British Columbia, CanadaElizabeth M. Simpson, B.Sc., M.Sc., Ph.D., is a leading scientist in mammalian genetics and genomics. The goal of her research is to improve treatment for human disorders of the brain and eye. Currently, she is focused on the development of gene-based delivery of therapy; also known as “gene therapy”. Dr Simpson has spearheaded multiple large international projects aimed at developing “MiniPromoters”, human DNA control elements that drive gene expression in regions of the brain and eye. The MiniPromoter technology is being used to enable gene therapy for treatment-resistant disorders such as Parkinson disease and Aniridia (congenital blindness). Dr Simpson is a Senior Scientist at the Centre for Molecular Medicine and Therapeutics (CMMT), a Professor at the University of British Columbia in the Department of Medical Genetics, and an Associate Member in the Departments of Psychiatry and Ophthalmology & Visual Sciences. She also directs the CMMT Mouse Animal Production Service (MAPS). |
|
| 10:00 - 10:10 | Discussion | |
| 10:10 - 10:30 |
Genome-wide CRISPR knockout screening to study protein quality control and neurodegeneration
The CRISPR associated Cas9 nuclease has emerged as an exciting new tool for genome-wide pooled forward genetic screens. In such experiments, the effect of knockout or activation of thousands of genes, on a specific cellular phenotype, can be measured in single experiments. Cas9 based screens displayed remarkable results including high perturbation efficiency, low off target effects and, most importantly, revealed a large number of previously uncharacterised validated gene hits when compared to previous methods. Dr Shalem will describe two approaches that are on-going in his lab and how they are using those to study genes that are implicated in neurodegenerative diseases: (1) Using selective vulnerability to identify mediators of protein homeostasis. (2) Combining endogenous gene tagging with fluorescence cell sorting based genome-wide screens to identify upstream regulators of protein expression, protein stability and protein aggregation. 
Dr Ophir Shalem, University of Pennsylvania and Children's Hospital of Philadelphia, USA

Dr Ophir Shalem, University of Pennsylvania and Children's Hospital of Philadelphia, USAOphir received a B.Sc. in computer science and computational biology from Beer Sheva University and a Ph.D. from the Weizmann institute of science. He then joined the lab of Professor Feng Zhang for his postdoctoral training where he was one of the pioneers in using CRISPR for genome-wide pooled functional screens. He spent the last year and a half of his postdoc as a visiting scholar in the lab of Andrew Dillin in UC Berkeley developing novel screening paradigms to study protein quality control pathways and neurodegenerative diseases in mammalian cell and animal models. Ophir opened his own lab at the University of Pennsylvania in September 2016 where he is continuing to use functional genomics approaches to study neurodegeneration. |
|
| 10:30 - 10:40 | Discussion | |
| 10:40 - 11:20 | Coffee | |
| 11:20 - 11:40 |
APP-overexpressing mice versus App knock-in mice for the preclinical studies of Alzheimer’s disease
Animal models of human diseases that recapitulate their pathology in an accurate manner represent indispensable tools for understanding molecular mechanisms and for use in preclinical studies. For more than two decades, the Alzheimer’s disease (AD) research community has depended on transgenic (Tg) mouse models that overexpress mutant amyloid precursor protein (APP) or APP and presenilin (PS), mutations of which cause familial AD (FAD). These mice exhibit the pathological hallmarks of AD, but it is becoming clear that the overexpression of transgenes from artificial promotors may cause phenotypes that may not related to AD. The next-generation mouse models contain humanized sequences and clinical mutations in the endogenous mouse App gene, leading to A accumulation without overexpression of APP or PS, avoiding at least these problems. Professor Saido will describe the different mouse models used to study AD including benefits and potential pitfalls. Professor Saido will then propose the broad adaptation of these models and the use of similar strategies to generate additional models for other neurodegenerative disorders. 
Professor Takaomi Saido , RIKEN Brain Science Institute, Japan

Professor Takaomi Saido , RIKEN Brain Science Institute, JapanTakaomi C. Saido (TCS) is a Senior Team Leader, Laboratory for Proteolytic Neuroscience, RIKEN Brain Science Institute. He received a PhD from Graduate School of Pharmaceutical Science, University of Tokyo, in 1988 and then became a Research Scientist at Tokyo Metropolitan Institute of Medical Science, where he mainly worked on the pathophysiology of calpain and on the pathological biochemistry of Alzheimer’s disease. After moving to RIKEN in 1997, he has continued to work both on calpain and Alzheimer’s disease. TCS identified the major A-degrading enzyme, neprilysin (Nat Med, 2000; Science, 2001; Lancet, 2003), and created the next-generation mouse models of Alzheimer’s disease (Nat Neurosci, 2014; J Neurosci, 2016). The calpastatin (CAST) knockout, conventional/conditional calpain 2 (CAPN2) knockout and single App knock-in mice generated in his laboratory are widely used in the research community. |
|
| 11:40 - 11:50 | Discussion | |
| 11:50 - 12:10 |
Working with complex mouse models to understand neurodegenerative disease

Dr Frances Wiseman, UCL Institute of Neurology, UK

Dr Frances Wiseman, UCL Institute of Neurology, UKFrances K. Wiseman was an undergraduate at the University of Oxford, UK, and completed her masters and Ph.D. at the University of Edinburgh, UK. Since 2007, she has been based at the Institute of Neurology, University College London, UK, studying the mechanisms that underlie the development of Alzheimer disease in people with Down syndrome. |
|
| 12:10 - 12:20 | Discussion | |
| 12:20 - 12:40 |
Improving validity of disease models through phenotype-driven approaches and changing genetic background
Precise genetic engineering of human disease-associated mutations into model organisms may not result in precise reproduction of the disease phenotype. This represents a conflict between face validity (does the model look right), and construct validity (does the phenotype develop for the right reason). The ultimate goal of a model is predictive validity (whether what we learn from the model translates to humans); however, the model’s acceptance will be greatest when face validity and construct validity align. Why an engineered model does not recapitulate the human disease phenotype is often unclear; however, these goals can sometimes be better aligned. First, phenotype-driven approaches to developing models start with good face validity, by definition. Such mutations have led to the identification of new human disease genes, or the identification of model-specific alleles with better face validity than precision engineered alleles. Second, genetic background almost invariably alters the phenotype in model organisms and in humans, resulting in variable severity, partial penetrance, and differing responses to treatment. We cannot always predict a sensitive or resistant strain background, but studying a given mutation on a variety of backgrounds can result in improved models. Furthermore, modifier loci can inform our understanding of disease mechanisms and therapeutic options. 
Dr Robert W. Burgess, The Jackson Laboratory, Bar Harbor, Maine, USA

Dr Robert W. Burgess, The Jackson Laboratory, Bar Harbor, Maine, USADr Burgess received his B.S. In Biochemistry and Physiology from Michigan State University, and his Ph.D. In Neuroscience from Stanford University. Following postdoctoral training at Washington University, St. Louis, Dr Burgess joined the faculty of The Jackson Laboratory in 2001. The Burgess lab seeks to understand the molecular mechanisms of synapse formation and maintenance at two sites in the nervous system: the peripheral neuromuscular junction and the retina. In all of these studies, we are addressing basic molecular mechanisms, but these basic mechanisms have relevance to human neuromuscular and neurodevelopmental disorders. Our continued research on the genetics underlying these disorders, and our continuing effort to identify new genes involved in these processes, will increase our understanding of the molecules required to form and maintain synaptic connectivity in the nervous system. |
|
| 12:40 - 12:50 | Discussion | |
| 12:50 - 13:00 |
Discussion: Tissue specificity, site of onset, time of onset, gain or loss of function

Professor Giampietro Schiavo, UCL Institue of Neurology, UK

Professor Giampietro Schiavo, UCL Institue of Neurology, UKProfessor Giampietro Schiavo obtained his PhD from the University of Padua, Italy, and received postdoctoral training at the Department of Biomedical Studies, University of Padua, Italy, and at the Memorial Sloan Kettering Cancer Center in New York, USA, under the supervision of Professors Cesare Montecucco and James Rothman, respectively. He was then recruited as junior group leader at the Cancer Research UK London Research Institute (then Imperial Cancer Research Fund), where he led the Molecular NeuroPathobiology Laboratory until 2013. He then moved to the Institute of Neurology at University College London as a full Professor in 2014. The goal of Professor Schiavo’s research is to understand the mechanisms underlying axonal retrograde transport how neurons control the uptake and sorting of ligands in health and disease conditions. |
Chair

Dr Pietro Fratta, UCL Institute of Neurology, UK

Dr Pietro Fratta, UCL Institute of Neurology, UK
| 14:00 - 14:20 |
Mouse physiology in modelling neurodegenerative disorders

Professor Linda Greensmith , UCL Institute of Neurology, UK

Professor Linda Greensmith , UCL Institute of Neurology, UKLinda Greensmith is recognised for her work on the pathophysiology of motor neuron degeneration, in particular in relation to motor neuron disorders (MNDs) such as Amyotrophic Lateral Sclerosis (ALS). She runs a large multidisciplinary research group at UCL Institute of Neurology, using a wide range of techniques, ranging from whole animal physiology to in vitro models. Linda’s interest in the neuromuscular system began with her doctoral thesis at UCL, examining the role of neuromuscular interactions in motor neuron development and survival. Between 1989-1996, Linda worked as a Postdoctoral Fellow, firstly at UCL and subsequently at Imperial College, where her research focused on motor neuron degeneration. In 1996 she was awarded a Wellcome Trust Fellowship to develop her skills in molecular biology and in 1999, Linda was awarded the prestigious Graham Watts Senior Research Fellowship at the UCL Institute of Neurology, funded by a bequest for MND Research at the Institute of Neurology. Since establishing the Graham Watts Laboratories, her group has grown and now has an international reputation in the field of MND and Neuromuscular Disorders. In particular, Linda is recognised for her expertise in mouse models of neuromuscular disease and for undertaking preclinical trials. In 2004, her laboratory made an important contribution to the field, identifying a novel co-inducer of protein chaperones as an effective neuroprotective agent for MND; Linda is a named inventor on the agent’s Patent. This work, published in Nature Medicine, has resulted in several international clinical trials. More recently, Linda has extended this work to show that targeting of protein chaperones may also have beneficial effects in the muscle disorder, inclusion body myositis. In a study published in Science Translational Medicine, using cellular and a mouse model of IBM, upregulation of the heat shock response was found to ameliorate the pathological signs and symptoms of IBM, and was found to be safe and well tolerated in a Phase IIa trial in IBM patients. In addition, in a study published in 2014 in Science, Linda has been developing a novel approach to restore function to paralysed respiratory muscles in MND patients. The approach combines optogenetics and regenerative medicine and uses stem cell-derived grafts of motoneurons that express channelrhodopsin-2, a molecular photo-sensor, to establish neuromuscular junctions with target muscles. Due to the photosensitivity of the graft, muscle contraction can then specifically be triggered by light flashes which are generated by an optical pacemaker device and transmitted to the graft via fiber optic cables. |
|
|---|---|---|
| 14:20 - 14:30 | Discussion | |
| 14:30 - 14:50 |
Understanding neuropathology in neurodegeneration models aligning human and mouse

Professor Maria Grazia Spillantini FMedSci FRS, University of Cambridge, UK

Professor Maria Grazia Spillantini FMedSci FRS, University of Cambridge, UKBorn in Arezzo (Italy), Maria Grazia Spillantini received a Laurea in Biological Sciences from Florence University and a PhD in Molecular Biology from Cambridge University working at the MRC Laboratory of Molecular Biology. In 1996 she moved to the Department of Clinical Neurosciences at Cambridge University, where she was first a Lecturer, then a Reader, and since 2007 Professor of Molecular Neurology. Her interest is on tauopathies and alpha-synucleinopathies. With her collaborators, she identified alpha-synuclein as the component of the filaments that form the Lewy bodies in Parkinson’s disease, dementia with Lewy bodies and the glial inclusions in multiple system atrophy and described one of the first mutations in the MAPT gene causing frontotemporal dementia. She has received several awards, including the Potamkin Prize and the Jay Van Andel award for achievements in Parkinson’s disease, the Thudicum Medal and the European Grand Prix of the French Foundation Recherce Alzheimer. She is a Fellow of the Royal Society, the Academy of Medical Sciences, Clare Hall (Cambridge) and Knight Officer of the Star of Italy. |
|
| 14:50 - 15:00 | Discussion | |
| 15:00 - 15:40 | Tea | |
| 15:40 - 16:00 |
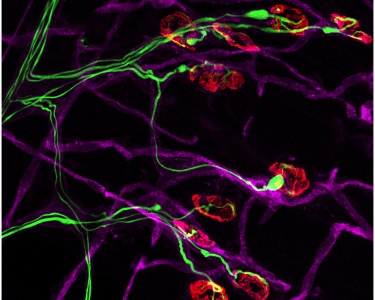
Mapping and manipulating neural circuits in vivo, possible applications in neurodegeneration models
Neural networks are emerging as the fundamental computational unit of the brain and it is becoming progressively clearer that network dysfunction is at the core of a number of psychiatric and neurodegenerative disorders. Yet, our ability to target specific networks for functional or genetic manipulations remains limited. Monosynaptically restricted Rabies virus facilitates the anatomical investigation of neural circuits. However, the inherent cytotoxicity of the Rabies largely prevents its implementation in long-term functional studies and for the genetic manipulation of neural networks. To overcome this limitation, we developed a Self-inactivating ΔG-Rabies virus (SiR) that transcriptionally disappears from the infected neurons while leaving permanent genetic access to the traced network. SiR provides a virtually unlimited temporal window for the genetic and functional manipulation of neural circuits in vivo without adverse effects on neuronal physiology and circuit function. 
Dr Marco Tripodi, MRC Laboratory of Molecular Biology, Cambridge, UK

Dr Marco Tripodi, MRC Laboratory of Molecular Biology, Cambridge, UKThe main aim of Dr Tripodi's research is to understand how neural circuits control movements. More recently he became interested in understanding the relationship between neuronal connectivity and neurodegenerative processes. After his MSc and PhD under the supervision of Michael Bate at the University Cambridge he became an EMBO fellow in the lab of Silvia Arber in Switzerland. In those years he implemented novel viral strategies to visualise and manipulate motor circuits in vivo, a research topic that he still actively pursues. In the autumn of 2013 he became junior group leader at the MRC Laboratory of Molecular Biology. |
|
| 16:00 - 16:10 | Discussion | |
| 16:10 - 16:30 |
Neuroimaging of mouse models
Imaging has revolutionised biomedical research over the past four decades, and innovations are continuing at an increasing pace. The immense challenge of annotating the entire mouse genome has led to the development of cutting-edge imaging tools in a drive to discover novel structural and functional information with a particular relevance to human pathobiology. Furthermore, sophisticated computational techniques are being combined with novel data acquisition for a deeper understanding of biological processes. This talk will include the latest neuroimaging developments, across a range of scales, in cellular and functional imaging using high-field MRI, Optical and Photoacoustic Imaging. I will introduce experimental optical techniques to image genes and function in mouse studies. As well as the development of new MRI methods to image glymphatic function, probe tissue microstructure, together with methods to image and guide therapies in vivo. 
Professor Mark Lythgoe , UCL Centre for Advanced Biomedical Imaging, UK

Professor Mark Lythgoe , UCL Centre for Advanced Biomedical Imaging, UKMark Lythgoe is Director of the UCL Centre for Advanced Biomedical Imaging (CABI), which is a multidisciplinary research centre for experimental imaging. The Centre hosts 12 state-of-the-art imaging modalities and 50 researchers. Professor Lythgoe is also Director of the Biological Imaging Research at the new Francis Crick Institute. Mark has a long-standing track record in the development of imaging techniques and has been awarded £43 million for his collaborative programme of research. He has published over 200 papers and has translated his research findings into clinical radiological practice. He founded the UCL Centre for Doctoral Training in Medical Imaging, which graduates around 15 PhD students each year, and is co-Director of the programme. Mark is also Chair of the Cheltenham Science Festival, and during his tenure it has become one of the largest science festivals in the world. |
|
| 16:30 - 16:40 | Discussion | |
| 16:40 - 17:00 |
Discussion: Differences in mouse versus humans, are we simply modelling mouse neurodegeneration?

Dr Pietro Fratta, UCL Institute of Neurology, UK

Dr Pietro Fratta, UCL Institute of Neurology, UK |
Chair

Professor Elizabeth Fisher, UCL Institute of Neurology, UK

Professor Elizabeth Fisher, UCL Institute of Neurology, UK
Elizabeth Fisher is Professor of Neurogenetics at University College London, in the Institute of Neurology, and focusses on genome engineering novel mouse models to understand neurodegenerative disease, specifically (1) aspects of human Down syndrome with respect to Alzheimer disease, and (2) forms of motor neuron degeneration largely related to amyotrophic lateral sclerosis. She joined UCL in 2001 and prior to that ran a lab at Imperial College London from 1990 to 2001. She was a postdoc at the Whitehead Institute at MIT (with David Page) from 1987 to 1990, having undertaken a PhD at Imperial College/MRC Harwell with Steve Brown and Mary Lyon. She has an undergraduate degree from the University of Oxford. EF was elected a Fellow of the Academy of Medical Sciences in 2007. In 2009 she became a Member of EMBO, and in 2010 became a Fellow of the Royal Society of Biology. She holds a Wellcome Trust Senior Investigators award jointly with Professor Victor Tybulewicz.
| 09:15 - 09:35 |
Molecular mechanisms of neurodegeneration - insights from cellular and in vitro models
Pathological protein aggregates are a central hallmark of all neurodegenerative diseases. In the related disorders ALS and FTD, the pathological aggregates consist mostly of the ubiquitous RNA-binding proteins TDP-43 or FUS. Both proteins are usually located in the nucleus, whereas in neurons and glial cells of ALS/FTD patients, they are partially lost from the nucleus and accumulate in large cytoplasmic inclusions. How TDP-43 mislocalization and aggregation arises in ALS/FTD patients is largely unclear. For FUS, we have successfully used cellular and in vitro models combined with neuropathological analysis of human post-mortem brains to identify two key pathomechanisms that appear to cause FUS mislocalization and aggregation in ALS or FTD patients: (1) In ALS-FUS, genetic mutations in the nuclear localization signal (NLS) of FUS cause impaired nuclear import of FUS, thus causing reduced nuclear and increased cytoplasmic FUS levels. This has recently been modelled in mice and was shown to cause age-dependent motor neuron degeneration1-3. However, no cytosolic FUS aggregates are found in these mice, suggesting that additional pathological hits / defects may be necessary to cause FUS aggregation in vivo. (2) In FTD-FUS patients the nuclear import receptor of FUS, Transportin, is aggregated and a post-translational modification of FUS, arginine methylation, is lost. Our recent in vitro work has shown that both defects promote pathological phase transitions and aggregation of FUS. The next challenge will be to model these defects in mice, in order to test whether they indeed cause FUS pathology and neurodegeneration in vivo. 
Dr Dorothee Dormann, Ludwig-Maximilians-University Munich, Germany

Dr Dorothee Dormann, Ludwig-Maximilians-University Munich, GermanyDr Dorothee Dormann studied Biochemistry in Tübingen, Germany and obtained a Ph.D. in Cell Biology/Immunology from the Rockefeller University, New York. In 2007, she joined the laboratory of Christian Haass at the LMU Munich as a postdoctoral fellow and started to investigate the cellular and molecular mechanisms that underlie the neurodegenerative diseases amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD). In 2014, she obtained the prestigious Heinz-Maier-Leibnitz Award and an Emmy-Noether-Fellowship of the German Research Foundation to start her independent group at the BioMedical Center of the LMU Munich. Her current research focuses on intracellular transport pathways of ALS/FTD-linked RNA-protein complexes and the mechanisms that lead to the pathological redistribution and aggregation of RNA-binding proteins, including FUS and TDP-43. |
|
|---|---|---|
| 09:35 - 09:45 | Discussion | |
| 09:45 - 10:05 |
Better modelling of human disease progression in mouse models - rationale and insights to be gained

Professor Karen Duff, Columbia University Medical Center, New York, USA

Professor Karen Duff, Columbia University Medical Center, New York, USADr Duff is professor of Pathology and Cell Biology and deputy director of the Taub institute at Columbia University Medical Center . After receiving her PhD from Sydney Brenner’s department at the University of Cambridge in 1991, she undertook postdoc positions in London with Alison Goate (1991-92) and John Hardy at the University of South Florida (1992-94). She joined the faculty at the University of South Florida then became an associate professor at Mayo Clinic in Florida. She joined the Nathan Kline Institute in New York in 1998, serving on the NYU faculty until joining Columbia in 2006. In her translational research program, Dr Duff has created several transgenic mouse models for Alzheimer’s disease to explore disease mechanisms and test therapeutic approaches. Her current interests are in exploring the role of the risk factor ApoE4 in AD pathogenesis, exploring the mechanisms and circuitry involved in spread of disease within the brain, and identifying the role and therapeutic potential of autophagy and proteasome-mediated clearance to remove pathological proteins. Dr Duff has published more than 120 peer-reviewed research articles and received a number of prizes, including the Potemkin Prize in 2005. |
|
| 10:05 - 10:15 | Discussion | |
| 10:15 - 10:35 |
Insights into the molecular basis of Huntington’s disease
Huntington’s disease (HD) is caused by a CAG/polyglutamine repeat expansion. HD research benefits from the availability of a wide-range of complementary mouse lines that model of aspects of the disease and have been validated in that they have predicted the presence of specific pathogenic processes in HD patients e.g. HTT aggregation and transcriptional dysregulation. HD mouse models are particularly useful for uncovering pathogenic mechanisms that lie proximal to the mutation. The group works with two versions of HD mice, those that are transgenic for a 5’ genomic fragment of HTT incorporating exon 1 (R6 lines), and with a range of knock-in models in which a CAG expansion has been inserted into mouse Htt. The molecular, behavioural, physiological and histological phenotypes of these two very different types of model are strikingly similar in symptomatic mice. This led us to discover that in all knock-in models, exon 1 does not always splice to exon 2 resulting in the presence of a small polyadenylated HTT mRNA that encodes the highly pathogenic exon 1 HTT protein. The R6 mouse lines are therefore a model of this incomplete splicing event, which has been subsequently shown to occur in HD patient post-mortem brain samples. 
Professor Gillian Bates, UCL Institute of Neurology, UK

Professor Gillian Bates, UCL Institute of Neurology, UKDr Gillian Bates is Professor of Molecular Neuroscience, co-Director of the Huntington’s Disease Centre and Vice Dean (Research), Faculty of Brain Sciences at UCL. During her postdoctoral work she was a key player in the team that, in 1993, cloned the Huntington’s disease gene. She developed the first mouse model of HD and her research programme is directed toward understanding the molecular basis of HD and validating therapeutic targets. She has been elected to the Academy of Medical Sciences (1999), European Molecular Biology Organisation (2002) and the Royal Society (2007). Prizes have included the Royal Society Glaxo Wellcome Award (with Stephen Davies) (1998), the Max Planck Research Award for International Cooperation (1999), the Klaus Joachim Zülch-Preis (2001) and the Leslie Brenner Gehry Prize for Innovation in Science (2011). |
|
| 10:35 - 10:45 | Discussion | |
| 10:45 - 11:15 | Coffee | |
| 11:15 - 11:35 |
Lost in translation: why do rodent models fail?
Rodent models of neuropsychiatric and neurodegenerative disorders are important experimental tools but their utility is often questioned. One area of particular concern is at the level of behavioural phenotyping. A key question is whether we are even studying the same psychological process(es) in rodents and humans, supported by the same neural circuits and structures. Memory impairment is a primary feature of many brain disorders and diseases, and is commonly assessed in rodent models using a wide variety of tasks. Many of the commonly used assays (e.g. watermaze, contextual fear, novel object recognition) are quick and easy to perform, but deficits are prone to misinterpretation and may not model the intended human phenotype. This will be illustrated with behavioural data from various mouse models of impaired neuroplasticity and calls for a more rigorous assessment of behavioural phenotypes in which psychological processes are identified across batteries of tests. Furthermore, I will describe a novel technique, tissue oxygen voltammetry (TOV) which measures the concentration of tissue oxygen in a given brain region in freely moving, behaving animals, and thus provides a haemodynamic signal of neural activity which is broadly analogous to the BOLD signal used in fMRI. TOV therefore represents an important approach for translating between rodent studies and humans in terms of identifying relevant neural circuits across species. 
Professor David Bannerman, University of Oxford, UK

Professor David Bannerman, University of Oxford, UKProfessor Bannerman obtained a B.Sc. (Hons.) degree in Pharmacology at the University of Bristol (1989) and a Ph.D. in Neuroscience at the University of Edinburgh (1995). He is Professor of Behavioural Neuroscience in the Department of Experimental Psychology at the University of Oxford (2010). His research is concerned with the neurobiological substrates of learning and memory, emotion and attention. In particular, studying the role of glutamate receptors and the hippocampus in memory and anxiety. |
|
| 11:35 - 11:45 | Discussion | |
| 11:45 - 12:05 |
Aligning mouse and human behaviours in neurodegeneration
Disruption to episodic memory is a major feature of the early stages of Alzheimer’s disease. Due to its historical association with episodic memory deficits in humans, the assessment of animal models of dementia has been largely hippocampus-centric. The use of ‘hippocampus-dependent’ tasks is common and assumes that this structure is central to memory dysfunction and that we fully understand its normal contribution to cognition. This is clearly not the case. Functional MRI imaging studies in human patients and those carrying risk genes for dementia, point to disruption not of an individual brain structure but of integrated networks that support memory – indeed some network changes may be present prior to manifestation of the clinical disease. A ‘one-structure’ approach to the assessment of animal models under estimates the impact of pathology and risk genes on the brain and it also restricts evaluation of potential therapies. In order to understand how ageing, genetic risk factors and core pathological changes eventually lead to progressive cognitive decline, an approach that focuses on the activity of integrated networks common to tasks in human and animals, may be very valuable. Such a strategy would promote harmonization of cognitive testing in rodents and humans and, ceteris paribus, enhance the translation of therapies. 
Professor Mark Good, Cardiff University, UK

Professor Mark Good, Cardiff University, UKProfessor Good undertook his undergraduate degree in Psychology at Goldsmiths College University of London and then a D.Phil under the supervision of Prof Euan Macphail at the University of York where he investigated cognitive functions of the avian hippocampus. He then undertook a postdoctoral position with Professor Richard Morris at the University of Edinburgh and subsequently a lectureship in the School of Psychology Cardiff University. Professor Good's research interests are concerned broadly with the neurobiology of learning and memory with a focus currently on using animal models of Alzheimer’s disease and Down syndrome to characterize cognitive, circuit and synaptic level activity in these disorders. |
|
| 12:05 - 12:15 | Discussion | |
| 12:15 - 12:30 |
Discussion: Transgenics or knock ins? Mouse paradigms or translating into human studies?

Professor Elizabeth Fisher, UCL Institute of Neurology, UK

Professor Elizabeth Fisher, UCL Institute of Neurology, UKElizabeth Fisher is Professor of Neurogenetics at University College London, in the Institute of Neurology, and focusses on genome engineering novel mouse models to understand neurodegenerative disease, specifically (1) aspects of human Down syndrome with respect to Alzheimer disease, and (2) forms of motor neuron degeneration largely related to amyotrophic lateral sclerosis. She joined UCL in 2001 and prior to that ran a lab at Imperial College London from 1990 to 2001. She was a postdoc at the Whitehead Institute at MIT (with David Page) from 1987 to 1990, having undertaken a PhD at Imperial College/MRC Harwell with Steve Brown and Mary Lyon. She has an undergraduate degree from the University of Oxford. EF was elected a Fellow of the Academy of Medical Sciences in 2007. In 2009 she became a Member of EMBO, and in 2010 became a Fellow of the Royal Society of Biology. She holds a Wellcome Trust Senior Investigators award jointly with Professor Victor Tybulewicz. |
Chair

Dr Pietro Fratta, UCL Institute of Neurology, UK

Dr Pietro Fratta, UCL Institute of Neurology, UK
| 13:30 - 13:50 |
The mouse toolbox we need for neurodegeneration - lessons from prion diseases

Professor John Collinge FRS, UCL Institute of Neurology, UK

Professor John Collinge FRS, UCL Institute of Neurology, UK |
|
|---|---|---|
| 13:50 - 14:00 | Discussion | |
| 14:00 - 14:20 |
What biopharma needs, what we do right and what we do wrong
The biopharma industry is in a unique position in the provision of healthcare. On the one hand, it can point to a range of stunning successes: very effective therapies for HIV, HCV, a pharmacological armamentarium trained against hypertension, diabetes and hypercholersterolaemia; personalized approaches for some tumours. On the other hand, a lack of success in providing true disease modifying therapeutics for Alzheimer’s disease and Parkinson’s disease. Dr Karran will examine those areas of scientific and operational strength that exist in pharma, and highlight some areas for future growth and development. 
Dr Eric Karran, Foundational Neuroscience Center, Cambridge, Massachusetts, USA

Dr Eric Karran, Foundational Neuroscience Center, Cambridge, Massachusetts, USAEric H. Karran PhD is a molecular biochemist by training. He is currently at AbbVie where he is Vice President, Distinguished Research Fellow and Site Head of the Foundational Neuroscience Center in Cambridge, Boston. Previously Eric was the Director of Research for Alzheimer’s Research UK. He has held senior positions in a number of companies, including SmithKline Beecham (now GSK), Pfizer, Eli Lilly and at Johnson and Johnson. Eric has specialized in Neuroscience research, particularly Alzheimer’s disease and other neurodegenerative diseases, for the past 20 years. Eric is a Visiting Professor in the Department for Human Genetics at the Catholic University of Leuven, Belgium; a Visiting Professor in the Department of Molecular Neuroscience at the Institute of Neurology, University College London; and Visiting Professor of Neurodegenerative Diseases at the University of Lincoln, United Kingdom. |
|
| 14:20 - 14:30 | Discussion | |
| 14:30 - 15:00 | Tea | |
| 15:00 - 15:20 |
Aiming for validity and reproducibility in mouse models of neurodegenerative disease
Pre-clinical studies using the mouse as a model for human disease have been criticized due to the failure of data to be replicated or to translate to the human. Common sources of error include bias in data analysis and reporting, as well as a failure to accurately report experimental conditions and controls. Neurodegenerative diseases present unique problems in disease modeling, perhaps because the lifespan of a mouse does not mimic that of a human. Overall, evidence that the mouse is a valid and predictive model of the human, and that the intervention targets similar molecules must be obtained prior to pre-clinical studies. Therefore, biomarkers and predictive assessments must be stringently defined. I will discuss model validity, predictive measurements, sources of experimental variation and their influence on phenotypic outcome using a mouse model for Rett syndrome as an archetype for preclinical studies. Here, understanding the differences presented by the animal model could be informative to human precision medicine. Therefore, perhaps the ultimate goal should not be to mimic the disease entirely as it presents in the human, but to aim to reveal mechanism, thereby informing disease and its treatment. 
Professor Monica Justice, SickKids, Toronto, Canada

Professor Monica Justice, SickKids, Toronto, CanadaDr Justice is a Senior Scientist and Head of the Program in Genetics and Genome Biology at The Hospital for Sick Children, and Professor of Molecular Genetics at the University of Toronto. A pioneer in mouse mutagenesis, Dr Justice’s research aims to improve human health through mouse genetics. Current work focuses on a genetic suppressor screen in a mouse model for Rett syndrome, which has unearthed new pathways for pathogenesis that suggest therapeutic entry points. She is Editor-in-Chief of Disease Models and Mechanisms, a Senior Editor of Current Protocols in Mouse Biology, a Fellow of the AAAS, and recipient of an American Cancer Society Junior Faculty Award, the Burroughs Wellcome Innovation Award in Functional Genomics, and the Michael E. DeBakey Excellence in Research Award. |
|
| 15:20 - 15:30 | Discussion | |
| 15:30 - 16:50 |
Modifier genes of neurodegeneration – a means to mechanism and new biology
To identify the underlying molecular causes of neurodegeneration, Professor Ackerman’s lab uses a forward genetic approach in mice. Importantly, this phenotype-driven approach allows the identification, without a priori assumptions, of molecules critical to these processes. However, the specific role of these molecules in neuronal homeostasis can be difficult to ascertain, particularly for molecules without defined function. To enable the definition of the biological pathways that when disrupted by mutations result in neurodegeneration, the lab has utilised forward genetics to identify modifier genes. In brief, the group analyses the consequences of alleles of various inbred mouse strains to identify genes which alter neuron death mediated by chemically-induced or spontaneous mutations. These modifier genes and the accompanying biochemical and genomic studies have helped pinpoint novel pathways involved in neuronal homeostasis in the ageing brain. 
Professor Susan Ackerman, University of California, USA

Professor Susan Ackerman, University of California, USADr Ackerman received her PhD from UCLA and was a postdoctoral fellow at University of Illinois Medical School and the Wistar Institute. Prior to her move to UCSD in 2016, Dr Ackerman was a Professor at The Jackson Laboratory in Bar Harbor, Maine, where she was a faculty member for nineteen years. She has been an Investigator of the Howard Hughes Medical Institute since 2005. Dr. Ackerman is working to identify and analyse the genes, pathways, and networks involved in the maintenance of neuronal homeostasis and age-related death of neurons in the central nervous system. |
|
| 15:50 - 16:00 | Discussion | |
| 16:00 - 16:20 |
Hallmarks of Alzheimer’s disease in stem cell-derived human neurons transplanted into mouse brain
Human pluripotent stem cells (PSC) provide a unique entry to study species-specific aspects of human disorders such as Alzheimer’s disease (AD). However in vitro culture of neurons deprives them of their natural environment. Here we transplanted human PSC-derived cortical neuronal precursors into the brain of a murine AD model. Human neurons differentiate and integrate into the brain, express 3R/4R Tau splice forms, show abnormal phosphorylation and conformational Tau changes and undergo neurodegeneration. Remarkably, cell death was dissociated from tangle formation in this natural 3D model of AD. Using genome wide expression analysis, we observed up-regulation of genes involved in myelination and down-regulation of genes related to memory and cognition, synaptic transmission and neuron projection. This novel chimeric model for AD displays human-specific pathological features and allows the analysis of different genetic backgrounds and mutations during the course of the disease. 
Professor Bart De Strooper, UK Dementia Research Institute, University College London, VIB and KU Leuven Belgium

Professor Bart De Strooper, UK Dementia Research Institute, University College London, VIB and KU Leuven BelgiumProfessor Bart De Strooper is the founding director of the UK Dementia Research Institute (UK DRI). He is a researcher in Alzheimer's disease, and supervises laboratories based in the UK DRI at the Francis Crick Institute in London and in the VIB laboratory at the KU Leuven in Belgium. Bart De Strooper’s research is focused on translating genetic findings into mechanisms of neurodegenerative diseases and drug targets. He is best known for his work on the presenilins and gamma-secretase, and more recently for his work on the cellular theory of Alzheimer’s Disease. He was elected to the Academy of Medical Sciences Fellowship in 2020, and has received several awards including the Potamkin prize, the Metlife Foundation Award for Medical Research, Alois Alzheimer’s prize, the highly prestigious Brain Prize 2018 and Commander in the Order of Leopold I.; |
|
| 16:20 - 16:30 | Discussion | |
| 16:30 - 17:00 |
Discussion: Differences in mouse versus humans, are we simply modelling mouse neurodegeneration?

Professor Giampietro Schiavo, UCL Institue of Neurology, UK

Professor Giampietro Schiavo, UCL Institue of Neurology, UKProfessor Giampietro Schiavo obtained his PhD from the University of Padua, Italy, and received postdoctoral training at the Department of Biomedical Studies, University of Padua, Italy, and at the Memorial Sloan Kettering Cancer Center in New York, USA, under the supervision of Professors Cesare Montecucco and James Rothman, respectively. He was then recruited as junior group leader at the Cancer Research UK London Research Institute (then Imperial Cancer Research Fund), where he led the Molecular NeuroPathobiology Laboratory until 2013. He then moved to the Institute of Neurology at University College London as a full Professor in 2014. The goal of Professor Schiavo’s research is to understand the mechanisms underlying axonal retrograde transport how neurons control the uptake and sorting of ligands in health and disease conditions. 
Professor Elizabeth Fisher, UCL Institute of Neurology, UK

Professor Elizabeth Fisher, UCL Institute of Neurology, UKElizabeth Fisher is Professor of Neurogenetics at University College London, in the Institute of Neurology, and focusses on genome engineering novel mouse models to understand neurodegenerative disease, specifically (1) aspects of human Down syndrome with respect to Alzheimer disease, and (2) forms of motor neuron degeneration largely related to amyotrophic lateral sclerosis. She joined UCL in 2001 and prior to that ran a lab at Imperial College London from 1990 to 2001. She was a postdoc at the Whitehead Institute at MIT (with David Page) from 1987 to 1990, having undertaken a PhD at Imperial College/MRC Harwell with Steve Brown and Mary Lyon. She has an undergraduate degree from the University of Oxford. EF was elected a Fellow of the Academy of Medical Sciences in 2007. In 2009 she became a Member of EMBO, and in 2010 became a Fellow of the Royal Society of Biology. She holds a Wellcome Trust Senior Investigators award jointly with Professor Victor Tybulewicz. 
Dr Pietro Fratta, UCL Institute of Neurology, UK

Dr Pietro Fratta, UCL Institute of Neurology, UK |
