Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Understanding the endosomal network in neurodegeneration
Online discussion meeting organised by Professor Peter Cullen, Professor Peter St George-Hyslop, Professor Scott Small and Dr Henne Holstege.
Abnormalities in the endosomal network are a signature feature of Alzheimer's disease, Parkinson's disease and numerous other neurological disorders. In bringing together world leading researchers from a range of disciplines, this meeting sought to discuss the latest advances in this rapidly moving field and foster collaborative efforts to enhance the rate of discovery in this medically important research field.
The schedule of talks and speaker biographies are available below. Speaker abstracts are also available below. This meeting had live closed captions.
Attending this event
This meeting has taken place.
Enquiries: contact the Scientific Programmes team
Schedule
| 10:00 - 10:05 | Introduction |
|---|---|
| 10:05 - 10:25 |
The role of AP-5/SPG15/SPG11 in endo-lysosomal homeostasis
Adaptor protein (AP) complexes are a family of evolutionarily ancient heterotetrameric complexes, which facilitate the transport of transmembrane cargo between membranes. AP-5 is the most recently discovered AP complex, and there is limited mechanistic understanding as to how and where it functions. AP-5 is stably associated with two additional proteins that are encoded by the SPG11 and SPG15 genes, and this association is essential for the stability and membrane association of the complex. Mutations in AP5Z1 (aka SPG48), SPG11 or SPG15 cause hereditary spastic paraplegia, pointing to an overall role of the AP-5 complex in neuronal maintenance and/or function. At the cellular level, electron microscopy of SPG48, SPG11 and SPG15 patient cell lines have revealed the accumulation of aberrant endolysosomes, pointing to a role for the AP-5 complex in the homeostasis of endosomes/lysosomes. The extreme low abundance of the AP-5 complex has hampered efforts to understand its localisation and membrane recruitment. The discovery that cells starved of nutrients enhance the recruitment of AP-5 to late endosomes/ lysosomes was a key finding that allowed a more thorough and systematic approach to understanding the mechanism. The recruitment of the AP-5 complex to membrane requires the coincidence detection of both a lipid (phosphatidylinositol 3-phosphate) and protein component (Rag GTPases), providing a rationale for the dynamic association of the AP-5 complex to late endosomes/lysosomes but also uncovering a link between the AP-5 complex and the mTORC1 nutrient-sensing pathway. 
Dr Jennifer Hirst, Cambridge Institute for Medical Research, UK

Dr Jennifer Hirst, Cambridge Institute for Medical Research, UKJennifer Hirst studied Biochemistry and Cell Biology in London before moving to the Cambridge Institute for Medical Research on the Cambridge Biomedical Campus. For the last 20 years she has been interested in the discovery and understanding of various intracellular sorting machineries that are necessary to deliver biologically important proteins to their correct destinations. She is currently focused on a complex comprised (in part) of the protein products of SPG48, SPG11, SPG15 (spastic paraplegia genes), where patients with defects in any of these components present with progressive neuropathy affecting principally the lower limbs. She utilises simple model tissue culture cells to provide a mechanistic understanding of the interplay of these proteins and the pathways that they act on, with a view to a wider understanding of what goes wrong in these conditions. |
| 10:25 - 10:45 |
Opposing functions for retromer and Rab11 in extracellular vesicle cargo traffic at presynaptic terminals
Neuronal extracellular vesicles (EVs) play critical roles in intercellular communication and in propagation of pathogenic proteins in neurological disease. However, little is known about how and where cargoes are selectively packaged into neuronal EVs. Here, we found that loss of the endosomal retromer complex leads to accumulation of the EV cargoes Amyloid Precursor Protein (APP) and Synaptotagmin-4 (Syt4) at presynaptic nerve terminals of Drosophila motor neurons, and increased release of these cargoes in EVs. Conversely, EV cargo levels are reduced in rab11 mutants, and EV cargo sorting depends on a balance between Rab11-mediated loading and retromer-dependent removal from EV precursor compartments. By systematically exploring known retromer-dependent trafficking mechanisms, we found that EV cargo regulation depends on the ESCPE-1 complex, and is separable from several other previously identified roles of neuronal retromer. Rab11 and retromer have previously been implicated in competing pathways in Alzheimer’s Disease, suggesting that they could serve as therapeutic targets for limiting accumulation and release of toxic EV cargoes. 
Professor Avital Rodal, Brandeis University, USA

Professor Avital Rodal, Brandeis University, USAAvital Rodal grew up in Ottawa, Canada. She attended MIT for her undergraduate studies in Biology and Chemical Engineering, and then University of California, Berkeley for her doctoral studies in Molecular and Cell Biology. She then did her postdoctoral work back at MIT, in the Picower Institute for Learning and Memory. She is currently an associate professor at Brandeis University, where she studies intracellular transport in neurons. She has been the recipient of NIH Pathway to Independence and NIH Director's New Innovator awards, a Pew scholar award, and recently the NINDS Landis Award for mentorship. |
| 10:45 - 11:05 |
Sorting nexin-27 regulates AMPA receptor trafficking through the synaptic adhesion protein LRFN2
The endosomal system is essential in controlling the transport of integral proteins and lipids (termed cargo) to a variety of cellular compartments, a function that is vital for cell survival. Recently, dysfunction of this system has been implicated as a key feature in the pathology of neurodegenerative disorders and many of the genes associated with familial forms of Parkinson’s and Alzheimer’s have been linked to the endosomal system. One of these genes VPS35 is a component of the retromer complex, which is important for regulating the retrieval, and trafficking of numerous cargoes away from the degradative pathway. In this talk Dr McMillan will focus on the retromer-associated cargo adaptor sorting nexin-27 (SNX27) which has been linked to various neuropathologies through the sorting of integral proteins to the synaptic surface, most notably AMPA receptors. The data suggest that SNX27 can control AMPA receptor-mediated synaptic transmission and plasticity indirectly through the endosomal sorting of a synaptic adhesion molecule LRFN2. Together, these data provide new molecular insight into the perturbed function of SNX27 and retromer in neurons and increases our understanding of how dysfunction of the endosomal network could lead to neurodegeneration. 
Dr Kirsty McMillan, University of Bristol, UK

Dr Kirsty McMillan, University of Bristol, UKThroughout her career Kirsty has developed a wide breadth of knowledge across biochemistry, neuroscience, and pharmacology to understand the molecular mechanisms driving neurodegeneration. Kirsty was awarded her BBSRC Industrial Collaborative PhD from the University of Bristol in Professor Maeve Caldwell’s lab in 2014. Her research investigated the role of microRNAs on the regulation of alpha synuclein expression. Since then, Kirsty has worked in the lab of Professor Peter Cullen at the University of Bristol, where she is currently a Research Fellow. Her research has focused on understanding the role of the endosomal system in neuronal and glial function, and in neurodegenerative disease. |
| 11:05 - 11:25 |
Endosomal coat assembly and regulation in neurodegeneration
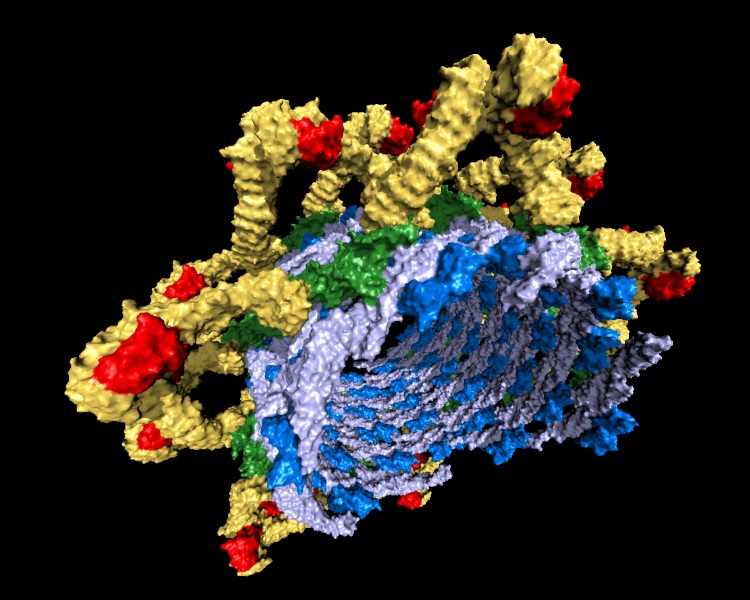
Mammalian retromer (VPS26/VPS35/VPS29 subunits) associates with sorting nexin (SNX) proteins to form coats on endosomal membranes and sort cargo proteins to the trans-Golgi network (TGN) or plasma membrane. This core heterotrimer complex is highly conserved from yeast to humans, but molecular mechanisms for mammalian retromer assembly and regulation remain undefined. Single particle cryoEM methods were used to resolve the first intact structures of mammalian retromer heterotrimer, and to identify the existence of multiple oligomers and longer flat chains in vitro. Comparisons with yeast SNX-BAR/retromer structures on membranes suggest retromer may function as an adaptable scaffold that is further ordered in the presence of cargoes, cargo adaptors, and/or regulators. Multiple small pharmacological chaperones have been shown to stabilize retromer structure and enhance its function, but precisely how and where they engage the complex remains unclear. Currently, a range of structural and biophysical methods are being employed to understand both how small molecules stabilize retromer and how regulators tune retromer function. A more complete molecular picture will enable the field to understand how retromer assembly is coupled to physiological function and may open exciting opportunities in translational research. 
Dr Lauren Parker Jackson, Vanderbilt University, USA

Dr Lauren Parker Jackson, Vanderbilt University, USALauren Jackson earned her bachelor of science (BS) degree in Chemistry (High Honors) with a Classical Studies minor at Vanderbilt University; she graduated summa cum laude as the College of Arts & Sciences Founders Medalist. She undertook PhD studies at the MRC Laboratory of Molecular Biology and Trinity College, University of Cambridge. She worked as a consultant at Boston Consulting Group (London) before completing postdoctoral training at the Cambridge Institute for Medical Research. Dr Jackson began her faculty appointment at Vanderbilt in 2014. Her work focuses on understanding molecular mechanisms that govern membrane trafficking pathways, especially how coat protein assembly and regulation drive fundamental cell biology and human disease. Dr Jackson’s research is supported by the Pew Charitable Trusts and NIH (NIGMS & NCI). She reviews for multiple funding bodies (NIH MBPP; Wellcome Trust; Medical Research Council; DFG) and journals (Nature Structural & Molecular Biology, eLife, Nature Chemical Biology, PNAS, J Biological Chemistry, J Cell Biology, Structure, Traffic, Wellcome Open). Dr Jackson is active in undergraduate biochemistry teaching. She received the Nordhaus Award for Excellence in Undergraduate Teaching (2019) and served as a Littlejohn Faculty Fellow in the Vanderbilt Undergraduate Summer Research Program. |
| 11:25 - 11:45 |
De novo macrocyclic peptides for inhibiting, stabilising and probing the function of the Retromer endosomal trafficking complex
The Retromer complex and associated sorting nexin (SNX) proteins are central mediators of endosomal membrane trafficking and signalling. In addition, mutations in Retromer can cause late-onset Parkinson’s disease, and Retromer can be hijacked by viral and bacterial pathogens during cellular infection. Seeking tools to modulate and probe Retromer function a series of de novo macrocyclic peptides have been discovered that bind to the trimeric Vps35-Vps26-Vps29 Retromer complex with high affinity and specificity. The majority of these cyclic peptides bind to a conserved surface on the Vps29 subunit. Crystal structures show that these peptides via use a di-peptide Pro-Leu sequence that structurally mimics other known interacting proteins including TBC1D5, VARP, and the bacterial effector RidL, and potently inhibit their association with Retromer in vitro and in cells. A unique macrocyclic peptide was found to bind Retromer at the interface between Vps35 and Vps26 subunits and can act as a potent molecular chaperone that stabilises the complex against thermal denaturation and disassembly. Importantly, binding of this peptide to Retromer does not perturb Retromer’s interaction with other essential regulatory proteins, and in fact allosterically enhances Retromer’s affinity for some proteins such as SNX27 and TBC1D5. Finally, its shown that the peptides can be used to probe the localisation and the proteome of Retromer interactions in cells. These macrocyclic peptides provide a potential toolbox for the study of Retromer and suggest new avenues for stabilising Retromer in future therapeutic approaches. 
Professor Brett Collins, The University of Queensland, Australia

Professor Brett Collins, The University of Queensland, AustraliaThe Collins lab is interested in understanding how molecular interactions between proteins and lipids control intracellular membrane trafficking, using structural biology and biophysical approaches. Current interests include (i) endosomal trafficking by the Retromer complex and the sorting nexin protein family, (ii) the formation of plasma membrane structures called caveolae, and (ii) the mechanisms of synaptic vesicle fusion controlled by SNARE proteins. After training at Macquarie University in Sydney with Professor Bridget Mabbutt and a postdoctoral period at the Cambridge Institute for Medical Research with Professor David Owen, Professor Collins returned to Australia in 2006 to take up an NHMRC RD Wright Career Development Award at the University of Queensland Institute for Molecular Bioscience. He currently holds an NHMRC Senior Research Fellowship and is head of the Molecular Trafficking lab at the IMB. Career highlights include determining the structure of the heterotetrameric AP2 complex that regulates receptor endocytosis at the plasma membrane (Cell, 2002, 2010), providing key insights into the Retromer transport assembly (Nature, 2018), defining a novel family of sorting nexin proteins that regulate endosomal sorting (Nat. Cell Biol. 2019, Nat. Struct. Mol. Biol, 2016), and providing the molecular insights into the assembly of caveolar membrane coat structures (Dev. Cell 2014; EMBO Rep, 2018). |
| 11:45 - 11:55 |
Selected short presentation
A novel role of presynaptic periactive zone proteins in extracellular vesicle trafficking Cassandra R Blanchette1, Amy L Scalera1, Zechuan Zhao1, Kathryn Harris2,3, Kate Koles1, Anna Yeh1, Julia K Apiki1, Bryan A Stewart2,3 and Avital A Rodal1 1Brandeis University, USA Extracellular vesicles (EVs) are small, endosomally-derived, membrane bound vesicles that mediate cell-cell communication in the healthy nervous system, as well as propagation of pathological proteins in neurodegenerative disease. However, it remains unclear how specific endosomal cargoes are sorted for release through the EV pathway. We identified an unexpected role for presynaptic periactive zone (PAZ) membrane remodeling proteins, which have canonical roles in clathrin-mediated endocytosis, in regulating the traffic of EV cargoes at presynaptic nerve terminals of Drosophila motor neurons. PAZ mutants, including those lacking synaptojanin, dynamin, endophilin, and the F-BAR/SH3 protein Nervous Wreck (Nwk) exhibit a local and dramatic decrease in the levels of the EV cargoes Synaptotagmin-4 (Syt4) and Amyloid Precursor Protein (APP) at presynaptic terminals. Further, this decrease is sufficient to abolish Syt4 function and reduce APP toxicity in the nervous system, suggesting that loss of specific EV cargoes may play unrecognized roles in canonical phenotypes of PAZ mutants. Interestingly, this novel EV cargo traffic defect is genetically separable from the well-established functions of these proteins in synaptic vesicle recycling and synaptic growth. Our data suggests a novel clathrin-dependent molecular mechanism that protects EV cargoes from local degradation at synapses, and promotes their release and function in EVs. |
| 11:55 - 12:05 |
Selected short presentation
Architecture of Retromer-SNX3 tubular coats and neurodegeneration-causing mutations Endosomes route trans-membrane cargo proteins either for degradation or to retrieval to the Golgi and cell surface. Retrieval defects lead to various pathophysiological conditions, including neurodegenerative disorders such as Alzheimer and Parkinson’s. The Retromer complex plays a key role in cargo retrieval. The hetero-trimeric VPS26/VPS29/VPS35 Retromer core associates with various sorting nexins (SNXs) including SNX-BARs and SNX3 to generate cargo-loaded tubular carriers that can be transported to destination compartments. Structural models are available for the fungal Retromer:SNX-BAR tubular coat, but it was unclear how Retromer could generate tubules without SNX-BARs. The group used cryo-electron tomography to study the reconstituted Retromer:SNX3-coated tubules of both metazoan and fungal origins. These coats display essentially identical architecture. They elucidated the structural basis of membrane remodelling and coupled cargo recognition, which are required for the formation of tubular carriers. These data provide the first glimpse of fully assembled cargo-containing metazoan Retromer coat. It also explains the causative mechanism of several neurodegeneration-linked mutations. |
Chair
Professor Margaret S Robinson FMedSci FRS, University of Cambridge, UK
Professor Margaret S Robinson FMedSci FRS, University of Cambridge, UK
Margaret Robinson received her PhD from Harvard University in 1982, then moved to the UK to take up a postdoctoral fellowship at the MRC Laboratory of Molecular Biology. In 1989 she moved to the Department of Clinical Biochemistry at the University of Cambridge as a Wellcome Trust Senior Research Fellow, in 1999 she became a Principal Research Fellow, and in 2003 she was appointed Professor of Molecular Cell Biology. She is currently based at the Cambridge Institute for Medical Research, where her lab works on membrane traffic and the role of coated vesicles. Her lab discovered or co-discovered the five adaptor protein complexes, including AP-4 and AP-5, which are mutated in certain forms of hereditary spastic paraplegia.
Professor Gregory Petsko, Harvard University and Cornell University, USA
Professor Gregory Petsko, Harvard University and Cornell University, USA
Gregory A Petsko is Professor of Neurology in the Ann Romney Center for Neurologic Diseases at Harvard Medical School and Brigham & Women’s Hospital in Boston, and Adjunct Professor of Biomedical Engineering at Cornell University. He has been elected to the National Academy of Sciences, the National Academy of Medicine, the American Academy of Arts and Sciences, and the American Philosophical Society. He is Past-President of the American Society for Biochemistry and Molecular Biology and of the International Union of Biochemistry and Molecular Biology. He has founded several publicly traded companies and serves on the advisory boards of MeiraGTx, Amicus Therapeutics, Proclara Biosciences, and Annovis Bio. His work aims to develop treatments for neurodegenerative diseases, including ALS, Alzheimer’s, and Parkinson’s. His public lectures on brain health have attracted a wide audience (one of his TED talks has been viewed over a million times). He has also written a widely-read column on science and society, the first ten years of which are available in book form. He admits, however, that the columns guest-written by his two dogs, Mink and Clifford, are more popular than those he writes himself.

Professor Peter Cullen, University of Bristol, UK

Professor Peter Cullen, University of Bristol, UK
Biography not available
| 13:00 - 15:00 |
Live panel discussion

Dr Jennifer Hirst, Cambridge Institute for Medical Research, UK

Dr Jennifer Hirst, Cambridge Institute for Medical Research, UKJennifer Hirst studied Biochemistry and Cell Biology in London before moving to the Cambridge Institute for Medical Research on the Cambridge Biomedical Campus. For the last 20 years she has been interested in the discovery and understanding of various intracellular sorting machineries that are necessary to deliver biologically important proteins to their correct destinations. She is currently focused on a complex comprised (in part) of the protein products of SPG48, SPG11, SPG15 (spastic paraplegia genes), where patients with defects in any of these components present with progressive neuropathy affecting principally the lower limbs. She utilises simple model tissue culture cells to provide a mechanistic understanding of the interplay of these proteins and the pathways that they act on, with a view to a wider understanding of what goes wrong in these conditions. 
Dr Lauren Parker Jackson, Vanderbilt University, USA

Dr Lauren Parker Jackson, Vanderbilt University, USALauren Jackson earned her bachelor of science (BS) degree in Chemistry (High Honors) with a Classical Studies minor at Vanderbilt University; she graduated summa cum laude as the College of Arts & Sciences Founders Medalist. She undertook PhD studies at the MRC Laboratory of Molecular Biology and Trinity College, University of Cambridge. She worked as a consultant at Boston Consulting Group (London) before completing postdoctoral training at the Cambridge Institute for Medical Research. Dr Jackson began her faculty appointment at Vanderbilt in 2014. Her work focuses on understanding molecular mechanisms that govern membrane trafficking pathways, especially how coat protein assembly and regulation drive fundamental cell biology and human disease. Dr Jackson’s research is supported by the Pew Charitable Trusts and NIH (NIGMS & NCI). She reviews for multiple funding bodies (NIH MBPP; Wellcome Trust; Medical Research Council; DFG) and journals (Nature Structural & Molecular Biology, eLife, Nature Chemical Biology, PNAS, J Biological Chemistry, J Cell Biology, Structure, Traffic, Wellcome Open). Dr Jackson is active in undergraduate biochemistry teaching. She received the Nordhaus Award for Excellence in Undergraduate Teaching (2019) and served as a Littlejohn Faculty Fellow in the Vanderbilt Undergraduate Summer Research Program. 
Professor Brett Collins, The University of Queensland, Australia

Professor Brett Collins, The University of Queensland, AustraliaThe Collins lab is interested in understanding how molecular interactions between proteins and lipids control intracellular membrane trafficking, using structural biology and biophysical approaches. Current interests include (i) endosomal trafficking by the Retromer complex and the sorting nexin protein family, (ii) the formation of plasma membrane structures called caveolae, and (ii) the mechanisms of synaptic vesicle fusion controlled by SNARE proteins. After training at Macquarie University in Sydney with Professor Bridget Mabbutt and a postdoctoral period at the Cambridge Institute for Medical Research with Professor David Owen, Professor Collins returned to Australia in 2006 to take up an NHMRC RD Wright Career Development Award at the University of Queensland Institute for Molecular Bioscience. He currently holds an NHMRC Senior Research Fellowship and is head of the Molecular Trafficking lab at the IMB. Career highlights include determining the structure of the heterotetrameric AP2 complex that regulates receptor endocytosis at the plasma membrane (Cell, 2002, 2010), providing key insights into the Retromer transport assembly (Nature, 2018), defining a novel family of sorting nexin proteins that regulate endosomal sorting (Nat. Cell Biol. 2019, Nat. Struct. Mol. Biol, 2016), and providing the molecular insights into the assembly of caveolar membrane coat structures (Dev. Cell 2014; EMBO Rep, 2018). 
Professor Avital Rodal, Brandeis University, USA

Professor Avital Rodal, Brandeis University, USAAvital Rodal grew up in Ottawa, Canada. She attended MIT for her undergraduate studies in Biology and Chemical Engineering, and then University of California, Berkeley for her doctoral studies in Molecular and Cell Biology. She then did her postdoctoral work back at MIT, in the Picower Institute for Learning and Memory. She is currently an associate professor at Brandeis University, where she studies intracellular transport in neurons. She has been the recipient of NIH Pathway to Independence and NIH Director's New Innovator awards, a Pew scholar award, and recently the NINDS Landis Award for mentorship. 
Dr Kirsty McMillan, University of Bristol, UK

Dr Kirsty McMillan, University of Bristol, UKThroughout her career Kirsty has developed a wide breadth of knowledge across biochemistry, neuroscience, and pharmacology to understand the molecular mechanisms driving neurodegeneration. Kirsty was awarded her BBSRC Industrial Collaborative PhD from the University of Bristol in Professor Maeve Caldwell’s lab in 2014. Her research investigated the role of microRNAs on the regulation of alpha synuclein expression. Since then, Kirsty has worked in the lab of Professor Peter Cullen at the University of Bristol, where she is currently a Research Fellow. Her research has focused on understanding the role of the endosomal system in neuronal and glial function, and in neurodegenerative disease. |
|---|
| 16:00 - 17:00 |
Early career 'table' discussions

Dr Jennifer Hirst, Cambridge Institute for Medical Research, UK

Dr Jennifer Hirst, Cambridge Institute for Medical Research, UKJennifer Hirst studied Biochemistry and Cell Biology in London before moving to the Cambridge Institute for Medical Research on the Cambridge Biomedical Campus. For the last 20 years she has been interested in the discovery and understanding of various intracellular sorting machineries that are necessary to deliver biologically important proteins to their correct destinations. She is currently focused on a complex comprised (in part) of the protein products of SPG48, SPG11, SPG15 (spastic paraplegia genes), where patients with defects in any of these components present with progressive neuropathy affecting principally the lower limbs. She utilises simple model tissue culture cells to provide a mechanistic understanding of the interplay of these proteins and the pathways that they act on, with a view to a wider understanding of what goes wrong in these conditions. 
Dr Lauren Parker Jackson, Vanderbilt University, USA

Dr Lauren Parker Jackson, Vanderbilt University, USALauren Jackson earned her bachelor of science (BS) degree in Chemistry (High Honors) with a Classical Studies minor at Vanderbilt University; she graduated summa cum laude as the College of Arts & Sciences Founders Medalist. She undertook PhD studies at the MRC Laboratory of Molecular Biology and Trinity College, University of Cambridge. She worked as a consultant at Boston Consulting Group (London) before completing postdoctoral training at the Cambridge Institute for Medical Research. Dr Jackson began her faculty appointment at Vanderbilt in 2014. Her work focuses on understanding molecular mechanisms that govern membrane trafficking pathways, especially how coat protein assembly and regulation drive fundamental cell biology and human disease. Dr Jackson’s research is supported by the Pew Charitable Trusts and NIH (NIGMS & NCI). She reviews for multiple funding bodies (NIH MBPP; Wellcome Trust; Medical Research Council; DFG) and journals (Nature Structural & Molecular Biology, eLife, Nature Chemical Biology, PNAS, J Biological Chemistry, J Cell Biology, Structure, Traffic, Wellcome Open). Dr Jackson is active in undergraduate biochemistry teaching. She received the Nordhaus Award for Excellence in Undergraduate Teaching (2019) and served as a Littlejohn Faculty Fellow in the Vanderbilt Undergraduate Summer Research Program. 
Professor Avital Rodal, Brandeis University, USA

Professor Avital Rodal, Brandeis University, USAAvital Rodal grew up in Ottawa, Canada. She attended MIT for her undergraduate studies in Biology and Chemical Engineering, and then University of California, Berkeley for her doctoral studies in Molecular and Cell Biology. She then did her postdoctoral work back at MIT, in the Picower Institute for Learning and Memory. She is currently an associate professor at Brandeis University, where she studies intracellular transport in neurons. She has been the recipient of NIH Pathway to Independence and NIH Director's New Innovator awards, a Pew scholar award, and recently the NINDS Landis Award for mentorship. 
Dr Kirsty McMillan, University of Bristol, UK

Dr Kirsty McMillan, University of Bristol, UKThroughout her career Kirsty has developed a wide breadth of knowledge across biochemistry, neuroscience, and pharmacology to understand the molecular mechanisms driving neurodegeneration. Kirsty was awarded her BBSRC Industrial Collaborative PhD from the University of Bristol in Professor Maeve Caldwell’s lab in 2014. Her research investigated the role of microRNAs on the regulation of alpha synuclein expression. Since then, Kirsty has worked in the lab of Professor Peter Cullen at the University of Bristol, where she is currently a Research Fellow. Her research has focused on understanding the role of the endosomal system in neuronal and glial function, and in neurodegenerative disease. |
|---|
| 10:00 - 10:20 |
Retromer-dependent traffic and tau secretion: mechanistic and therapeutic implications
Retromer is the dominant trafficking complex that recycles cargo out of endosomes. Retromer was first linked to Alzheimer’s disease by expression profiling studies that set out to understand why the entorhinal cortex is differentially vulnerable to the disease. Since then many studies have established a mechanistic link to Alzheimer’s disease. By using manipulations that either decrease or increase retromer recycling in model systems, retromer has been shown to mediate the disease’s four core pathologies: Amyloid pathology, tau pathology, synaptic pathology, and microglia pathology. While retromer recycling defects exist in, and are pathogenically linked, to the disease, the frequency of retromer dysfunction remains unknown. To address this question, the group set out to identify a biomarker of retromer dysfunction in the cerebrospinal fluid (CSF). They began by genetically-engineering a mouse to have retromer dysfunction selectively in forebrain neurons. A proteomic screen of CSF and subsequent validation studies showed that retromer dysfunction is associated with CSF elevations of APLP1, CHL1, and the microtubule binding protein tau. Next, the group turned to human studies, and developed new assays that allow them to reliably measure all three proteins in human CSF. By establishing the relationship of all three proteins in the CSF of healthy controls and Alzheimer patients in the dementia and prodromal stages disease, the results suggest that retromer recycling dysfunction might exist in a majority of patients. These findings have both mechanistic and therapeutic implications. 
Professor Scott Small, Columbia University, USA
Professor Scott Small, Columbia University, USAScott A. Small MD is the Director of the Alzheimer’s Disease Research Center at Columbia University, where he also directs the Psychosis Research Program. Dr. Small focuses on disorders that affect the hippocampus, a brain structure targeted by Alzheimer’s disease, schizophrenia, and the normal wear & tear of the aging process. The hippocampus is a circuit comprised of a handful of microscopic regions. The overarching hypothesis motivating Dr. Small’s lab is that if hippocampal regions most vulnerable to a disorder can be pinpointed, this anatomical information can guide a search for the disorder’s root cause. Accordingly, Dr. Small’s ‘anatomical biology’ lab has pioneered the development of MRI tools best suited to isolate vulnerable hippocampal regions. His lab has then used this information to identify mechanisms that are now thought to underlie Alzheimer’s disease, schizophrenia, and ‘cognitive aging’. Most recently, his lab has begun developing interventions for each condition. To date, the lab has completed two clinical trials for cognitive aging and one for schizophrenia, and the lab’s Alzheimer’s disease findings was the cornerstone around which a new biotechnology company, Retromer Therapeutics. was formed. |
|---|---|
| 10:20 - 10:40 |
Roles of the endo-lysosomal system in dementia initiation and pathogenesis
Endolysosome dysfunction is emerging as an important pathogenic process in many neurodegenerative diseases, including Alzheimer’s disease, frontotemporal dementia, and lysosomal storage disorders. Using human stem cell-derived neurons, the group has found that autosomal dominant mutations in PSEN1, APP and SORL1 causal for Alzheimer’s disease all cause defects in human neuronal endolysosome function, compromising the degradative phase of autophagy. Furthermore, the proteins encoded by all three genes are localised to the endolysosomal network and act in a single pathway to regulate endolysosome function. Endolysosome dysfunction occurs in young neurons, prior to any protein aggregation, affecting endosome size and number, lysosome transport to the neuronal cell body, lysosome maturation (reflected in protease activation) and lysosome function in the degradative phase of autophagy, indicating that endolysosome dysfunction is a primary pathogenic effect of monogenic AD mutations in these genes. Tauopathies, including AD, share a feature of apparent spatial spreading through neural networks, from affected to healthy neurons. Whole genome CRISPR screens in human neurons were used to identify genes and pathways required for neuronal uptake of both monomeric and aggregated tau. In addition to key surface receptors and receptor-mediated endocytosis, those screens found that disruption of different aspects of intracellular vesicular trafficking alters tau uptake, pointing to roles for the endolysosomal system in both neurodegenerative disease initiation and progression. 
Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UK

Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UKRick Livesey is Professor of Stem Cell Biology at the UCL/Great Ormond Street Institute of Child Health. He is also head of the Genetic and Neurodevelopmental Disorders Research Unit at Biogen, and scientific founder of two biotech spinouts based in Cambridge, Talisman Therapeutics and Gen2 Neuroscience. Prior to joining UCL in 2018, he was a Senior Group Leader at the Wellcome Trust/Cancer Research UK Gurdon Institute at the University of Cambridge. His research focuses on the cell and molecular biology of neurodegenerative disease, with particular interest in genetic diseases of the cerebral cortex in children and adults and the development of novel therapeutics for those conditions.
|
| 10:40 - 11:00 |
Dynein promotes retrograde transport of late endosomes in dendrites and is required for degradation of somatodendritic cargos
Unlike axons, dendrites in vertebrate neurons have microtubule arrays with mixed polarities. The question of how directional transport is organised in dendrites is thus a longstanding one. Dynein has been reported as either an anterograde or retrograde motor in dendrites. The group has studied endosomal transport in dendrites, in particular the trafficking of the neuronal dendritic membrane proteins NSG1/2. They previously found that NSG1/2 was endocytosed into dendritic early endosomes and then rapidly transported via late endosomes to the soma where most of the lysosomes reside. When Rab7 function was impaired by expression of Rab7-T22N, late endosomes carrying endocytosed NSG1/2 stopped moving and accumulated high levels of NSG1/2 throughout dendrites. The group now asks if movement of late endosomes towards the soma requires kinesin or dynein motors. Since the retrograde transport and subsequent degradation of NSG1/2 depended on Rab7, they first expressed two Rab7 effectors, FYCO1 which recruits kinesin and moves lysosomes to the cell periphery in fibroblasts, and RILP which recruits dynein and moves lysosomes to the cell centre in fibroblasts. RILP overexpression leads to massive re-localisation of late endosomes to the soma whereas FYCO1 overexpression does not. This observation suggests that dynein promotes retrograde movement of late endosomes in dendrites. In order to test this hypothesis more directly, the group carried out live imaging of Rab7-mCherry. Overexpression of DIC2-GFP leads to an increase in net retrograde movements of Rab7-positive compartments, but anterograde discursions are frequent as well. In addition, they live imaged Rab7-mCherry in the presence of dynein inhibitors (CC1-GFP, ciliobrevin). Both of these approaches largely halt Rab7 movements in dendrites. The group then determined if degradation of NSG1/2 was slowed if dynein function is disrupted with CC1 overexpression. They find that NSG1/2 accumulates in dispersed compartments in dendrites and degradation is slowed. In addition, they find reduced accumulation of acidified (Lysotracker-positive) compartments in somata of CC1-GFP expressing neurons. Lastly, DQ-BSA conversion to red (a degradative tracer) is reduced in the somata of CC1-GFP expressing neurons. These data show that late endosomes use dynein motors for net motility to the soma and thus use dendritic plus end-out microtubules as their tracks for motility. 
Dr Bettina Winckler, University of Virginia Medical School, USA

Dr Bettina Winckler, University of Virginia Medical School, USABettina Winckler was trained as a cell biologist in Dr Frank Solomon's lab at MIT where she received a PhD in 1994. She subsequently trained as a postdoc with Dr Ira Mellman and Dr Mu-ming Poo. She started her own lab in 2000 at Mount Sinai School of Medicine in New York and moved to the University of Virginia where she is Full Professor in the Department of Cell Biology. Dr Winckler has long-standing interests in how cells elaborate and maintain polarized morphologies, with a focus on neurons. Her work investigates the regulation of the endosomal pathway in dendrites in time and space. Currently, her lab is studying the transport of short-lived dendritic membrane proteins to somatic lysosomes and the regulation by Rab7 and its effectors. A second interest of the Winckler lab is the elucidation of novel signalling roles of intermediate filaments in neurons. |
| 11:00 - 11:20 |
The impact of SORL1 loss on endo-lysosomal network function in human CNS cells
Enlarged early endosomes, indicative of endosomal traffic jams, are a hallmark cytopathology in Alzheimer’s Disease. The sorting receptor SorLA, encoded by the established risk gene SORL1, has a defined role in endolysosomal trafficking of the amyloid precursor protein, APP. Research in the Young lab has demonstrated that loss of SORL1 in hiPSC-derived neurons leads to enlarged early endosomes in an amyloid-independent manner and that this endosome enlargement can be rescued by treatment with retromer-stabilizing molecules. Further work in the lab shows that modulation of SORL1 expression affects the sorting of neuronal cargo other than APP, and functionally demonstrates a role for SORL1 in lysosomal trafficking in both hiPSC-derived neurons and microglia. RNA-seq analysis of SORL1 deficient neurons indicates altered expression and network interaction changes in neurotrophin and synaptic genes, demonstrating that endosomal traffic jams induced by loss of SORL1 impair pathways necessary for neuronal health and function. Collectively, these studies suggest that SORL1 plays multiple roles in central nervous system cells and that strategies enhancing endosomal trafficking should be considered as therapeutic targets for AD. 
Dr Jessica Young, University of Washington, USA

Dr Jessica Young, University of Washington, USAJessica Young received her PhD in Molecular and Cell Biology in 2009 from the University of Washington in the laboratory of Dr Albert La Spada where she studied the role of autophagy in neurodegenerative disease. She pursued postdoctoral training with Dr Lawrence SB Goldstein at the University of California, San Diego where she focused on developing human induced pluripotent stem cell (hiPSC) models of Alzheimer’s disease. She is currently an Assistant Professor in the Department of Laboratory Medicine and Pathology at the University of Washington where, since 2016, her laboratory is working to understand the role of AD risk genes in neuronal endo-lysosomal dysfunction using patient derived and gene-edited hiPSCs. The Young lab is dedicated to building accurate in vitro models of neurodegenerative disease and understanding cell biological mechanisms the lead to disease pathogenesis. Current funded projects in the lab include 1) understanding the role of SORL1 in endo-lysosomal trafficking in hiPSC-derived neurons, microglia, and brain organoids and 2) elucidating epigenetic mechanisms that regulate neuronal metabolism and ageing. Dr Young’s research is funded by the BrightFocus Foundation and the NIH (NIA). |
| 11:20 - 11:40 |
Endosomal trafficking is required for the normal maturation of the Alzheimer’s-associated protein SORLA
SORL1 is among the most significant genetic factors that affect development of Alzheimer’s disease (AD). This gene encodes a sorting receptor, SORLA, involved in trafficking of multiple different cargoes between cell surface and golgi/endosomal compartments. SORLA undegoes posttranslational modifications and maturation with ultimate ectodomain shedding, however knowledge of these processes remains limited. Here it is demonstrated that SORLA exists in two forms at the plasma membrane, an immature and a mature form, characterised by distinct N-glycosylation profiles. The mature receptor form is shed from the cell surface, whereas immature form of sorLA does not undergo shedding. Conversion of the immature to the mature N-glycan profile relies on endocytosis and recycling of the receptor to the cell surface by a retromer-dependent endosomal trafficking pathway. Understanding the maturation process of SORLA has implications for assessment of genetic SORL1 variants identified in AD patients, as mutations that cause misfolding or trafficking dysfunction are likely to impair maturation. Therefore, the data presented point to impaired maturation as a signature of AD-associated SORLA dysfunction. This can be utilised for future functional studies to assess pathogenicity of genetic SORL1 variants. 
Dr Olav Andersen, Aarhus University, Denmark

Dr Olav Andersen, Aarhus University, DenmarkOlav Andersen graduated from Aarhus University in 2001, followed by 6 years as postdoctoral researcher at the Max-Delbrück-Center for molecular medicine in Berlin, before he returned to Aarhus University to become associate professor and establishing his research group focusing on SORL1 and Alzheimer’s disease. |
| 11:40 - 11:50 |
Selected short presentation
Regulation of lipid trafficking at endoplasmic reticulum-plasma membrane contact sites in photoreceptor neurons Bishal Basak, Harini Krishnan and Padinjat Raghu At the distal regions of neurons, vesicular trafficking is inefficient to maintain lipid homeostasis. Instead, the cell relies on contacts formed between closely apposed organellar membranes for lipid transfer. Perturbations of contacts formed between the endoplasmic reticulum [ER] and mitochondria have been implicated in neurodegeneration. However, the mechanisms by which these contact sites directly contribute to maintaining neuronal physiology remain unclear. Drosophila photoreceptors are morphologically polarized neurons forming contacts between the apical plasma membrane [PM] and ER, which are indispensable for maintaining cellular integrity. RDGB is a key protein that tightly controls this process by transferring phospholipids at the contact sites, which in turn is essential to maintain organellar lipid homeostasis. Electrophysiological recordings from photoreceptors devoid of RDGB function show significant reduction in light response and sensitivity, subsequently leading to retinal degeneration. This study demonstrates that the function of RDGB at the ER-PM junction depends on interaction with phospholipids at the PM and also with the integral ER protein, VAP. Additionally, inter-domain movements within the RDGB protein directly regulate its lipid transfer function. Disruption of these interactions severely impacts lipid homeostasis leading to photoreceptor degeneration. Thus, this study provides insight into how regulation of lipid transfer is fine-tuned to maintaining neuronal structure and function. |
| 11:50 - 12:00 |
Selected short presentation
TMCC2, an endosomal/ER protein that differentially interacts with isoforms of apolipoprotein E and the Amyloid Precursor Protein associated with Alzheimer’s Disease Paul CR Hopkins, Michelle Lupton, Richard Killick, John Hardy, John Powell and Guy Tear Transmembrane and Coiled-Coil 2 (TMCC2) is a protein that regulates endosome fission at the ER, and forms complexes with both apolipoprotein E (apoE) and the Amyloid Precursor Protein (APP). TMCC2 demonstrates isoform-specific interactions, interacting differentially with risk versus normal forms of both proteins. TMCC2 is a member of a highly evolutionarily conserved gene family; the Drosophila orthologue (called Dementin) is essential for brain development, modifies metabolism of the APP-Like protein in vivo and protects against mis-expression of human APP. Dementin alleles cause neurodegeneration with features of Alzheimer’s disease (AD), ie accumulation of fragments of the APP-Like protein, defects in synaptogenesis, cellular mis-localization of microtubule-binding proteins and early death. The group performed targeted exome sequencing of TMCC2 in AD cases and controls and found an excess of TMCC2 variants in AD cases. Several of these had modified activity towards apoE and APP that affected the amount of Aβ secreted from cultured human cells. TMCC2 is abundantly expressed in the human brain where anti-TMCC2 antibodies detect a primarily neuronal expression pattern. TMCC2 may thus act to link apoE isoforms and APP to defects of the endo-lysosomal system in AD. |
Chair

Dr Katrin Deinhardt, University of Southampton, UK

Dr Katrin Deinhardt, University of Southampton, UK
Dr Katrin Deinhardt in an Associate Professor in Neuroscience at the University of Southampton. She received her first degree in biochemistry at the Freie Universität Berlin and a PhD in cell biology at Cancer Research UK (through UCL). Following her postdoctoral studies at the Skirball Insitute (New York University) she established her independent research group at the School of Biological Sciences, University of Southampton in 2013. Katrin’s research interest focuses on the interactions between membrane trafficking and cellular signalling that regulate neuronal structural maintenance in health and disease.

Professor Stéphane Lefrançois, INRS, Canada

Professor Stéphane Lefrançois, INRS, Canada
Stéphane Lefrançois obtained his BSc and PhD at McGill University in Montreal before undertaking post-doctoral training at the National Institutes of Health (NIH) in Bethesda, MD. He was subsequently recruited in 2007 to the Université de Montréal, before joining the Institut national de la recherche scientifique (INRS) in 2015. He is currently an associate professor at INRS and his laboratory is located at Centre Armand-Frappier Santé Biotechnologie. Professor Lefrançois’ research interests include the regulation of intracellular trafficking by post-translational modifications with a focus on endosomal sorting, and determining the molecular function of the endolysosomal proteins CLN3 and CLN5. Mutations in these proteins cause Neuronal Ceroid Lipofuscinosis, a rare neurodegenerative disease that mainly affects children.
| 13:00 - 15:00 |
Live panel discussion

Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UK

Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UKRick Livesey is Professor of Stem Cell Biology at the UCL/Great Ormond Street Institute of Child Health. He is also head of the Genetic and Neurodevelopmental Disorders Research Unit at Biogen, and scientific founder of two biotech spinouts based in Cambridge, Talisman Therapeutics and Gen2 Neuroscience. Prior to joining UCL in 2018, he was a Senior Group Leader at the Wellcome Trust/Cancer Research UK Gurdon Institute at the University of Cambridge. His research focuses on the cell and molecular biology of neurodegenerative disease, with particular interest in genetic diseases of the cerebral cortex in children and adults and the development of novel therapeutics for those conditions.

Dr Bettina Winckler, University of Virginia Medical School, USA

Dr Bettina Winckler, University of Virginia Medical School, USABettina Winckler was trained as a cell biologist in Dr Frank Solomon's lab at MIT where she received a PhD in 1994. She subsequently trained as a postdoc with Dr Ira Mellman and Dr Mu-ming Poo. She started her own lab in 2000 at Mount Sinai School of Medicine in New York and moved to the University of Virginia where she is Full Professor in the Department of Cell Biology. Dr Winckler has long-standing interests in how cells elaborate and maintain polarized morphologies, with a focus on neurons. Her work investigates the regulation of the endosomal pathway in dendrites in time and space. Currently, her lab is studying the transport of short-lived dendritic membrane proteins to somatic lysosomes and the regulation by Rab7 and its effectors. A second interest of the Winckler lab is the elucidation of novel signalling roles of intermediate filaments in neurons. 
Dr Olav Andersen, Aarhus University, Denmark

Dr Olav Andersen, Aarhus University, DenmarkOlav Andersen graduated from Aarhus University in 2001, followed by 6 years as postdoctoral researcher at the Max-Delbrück-Center for molecular medicine in Berlin, before he returned to Aarhus University to become associate professor and establishing his research group focusing on SORL1 and Alzheimer’s disease. 
Dr Jessica Young, University of Washington, USA

Dr Jessica Young, University of Washington, USAJessica Young received her PhD in Molecular and Cell Biology in 2009 from the University of Washington in the laboratory of Dr Albert La Spada where she studied the role of autophagy in neurodegenerative disease. She pursued postdoctoral training with Dr Lawrence SB Goldstein at the University of California, San Diego where she focused on developing human induced pluripotent stem cell (hiPSC) models of Alzheimer’s disease. She is currently an Assistant Professor in the Department of Laboratory Medicine and Pathology at the University of Washington where, since 2016, her laboratory is working to understand the role of AD risk genes in neuronal endo-lysosomal dysfunction using patient derived and gene-edited hiPSCs. The Young lab is dedicated to building accurate in vitro models of neurodegenerative disease and understanding cell biological mechanisms the lead to disease pathogenesis. Current funded projects in the lab include 1) understanding the role of SORL1 in endo-lysosomal trafficking in hiPSC-derived neurons, microglia, and brain organoids and 2) elucidating epigenetic mechanisms that regulate neuronal metabolism and ageing. Dr Young’s research is funded by the BrightFocus Foundation and the NIH (NIA). 
Professor Scott Small, Columbia University, USA
Professor Scott Small, Columbia University, USAScott A. Small MD is the Director of the Alzheimer’s Disease Research Center at Columbia University, where he also directs the Psychosis Research Program. Dr. Small focuses on disorders that affect the hippocampus, a brain structure targeted by Alzheimer’s disease, schizophrenia, and the normal wear & tear of the aging process. The hippocampus is a circuit comprised of a handful of microscopic regions. The overarching hypothesis motivating Dr. Small’s lab is that if hippocampal regions most vulnerable to a disorder can be pinpointed, this anatomical information can guide a search for the disorder’s root cause. Accordingly, Dr. Small’s ‘anatomical biology’ lab has pioneered the development of MRI tools best suited to isolate vulnerable hippocampal regions. His lab has then used this information to identify mechanisms that are now thought to underlie Alzheimer’s disease, schizophrenia, and ‘cognitive aging’. Most recently, his lab has begun developing interventions for each condition. To date, the lab has completed two clinical trials for cognitive aging and one for schizophrenia, and the lab’s Alzheimer’s disease findings was the cornerstone around which a new biotechnology company, Retromer Therapeutics. was formed. |
|---|
| 16:00 - 17:00 |
Early career 'table' discussions

Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UK

Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UKRick Livesey is Professor of Stem Cell Biology at the UCL/Great Ormond Street Institute of Child Health. He is also head of the Genetic and Neurodevelopmental Disorders Research Unit at Biogen, and scientific founder of two biotech spinouts based in Cambridge, Talisman Therapeutics and Gen2 Neuroscience. Prior to joining UCL in 2018, he was a Senior Group Leader at the Wellcome Trust/Cancer Research UK Gurdon Institute at the University of Cambridge. His research focuses on the cell and molecular biology of neurodegenerative disease, with particular interest in genetic diseases of the cerebral cortex in children and adults and the development of novel therapeutics for those conditions.

Dr Bettina Winckler, University of Virginia Medical School, USA

Dr Bettina Winckler, University of Virginia Medical School, USABettina Winckler was trained as a cell biologist in Dr Frank Solomon's lab at MIT where she received a PhD in 1994. She subsequently trained as a postdoc with Dr Ira Mellman and Dr Mu-ming Poo. She started her own lab in 2000 at Mount Sinai School of Medicine in New York and moved to the University of Virginia where she is Full Professor in the Department of Cell Biology. Dr Winckler has long-standing interests in how cells elaborate and maintain polarized morphologies, with a focus on neurons. Her work investigates the regulation of the endosomal pathway in dendrites in time and space. Currently, her lab is studying the transport of short-lived dendritic membrane proteins to somatic lysosomes and the regulation by Rab7 and its effectors. A second interest of the Winckler lab is the elucidation of novel signalling roles of intermediate filaments in neurons. 
Dr Olav Andersen, Aarhus University, Denmark

Dr Olav Andersen, Aarhus University, DenmarkOlav Andersen graduated from Aarhus University in 2001, followed by 6 years as postdoctoral researcher at the Max-Delbrück-Center for molecular medicine in Berlin, before he returned to Aarhus University to become associate professor and establishing his research group focusing on SORL1 and Alzheimer’s disease. 
Dr Jessica Young, University of Washington, USA

Dr Jessica Young, University of Washington, USAJessica Young received her PhD in Molecular and Cell Biology in 2009 from the University of Washington in the laboratory of Dr Albert La Spada where she studied the role of autophagy in neurodegenerative disease. She pursued postdoctoral training with Dr Lawrence SB Goldstein at the University of California, San Diego where she focused on developing human induced pluripotent stem cell (hiPSC) models of Alzheimer’s disease. She is currently an Assistant Professor in the Department of Laboratory Medicine and Pathology at the University of Washington where, since 2016, her laboratory is working to understand the role of AD risk genes in neuronal endo-lysosomal dysfunction using patient derived and gene-edited hiPSCs. The Young lab is dedicated to building accurate in vitro models of neurodegenerative disease and understanding cell biological mechanisms the lead to disease pathogenesis. Current funded projects in the lab include 1) understanding the role of SORL1 in endo-lysosomal trafficking in hiPSC-derived neurons, microglia, and brain organoids and 2) elucidating epigenetic mechanisms that regulate neuronal metabolism and ageing. Dr Young’s research is funded by the BrightFocus Foundation and the NIH (NIA). 
Professor Scott Small, Columbia University, USA
Professor Scott Small, Columbia University, USAScott A. Small MD is the Director of the Alzheimer’s Disease Research Center at Columbia University, where he also directs the Psychosis Research Program. Dr. Small focuses on disorders that affect the hippocampus, a brain structure targeted by Alzheimer’s disease, schizophrenia, and the normal wear & tear of the aging process. The hippocampus is a circuit comprised of a handful of microscopic regions. The overarching hypothesis motivating Dr. Small’s lab is that if hippocampal regions most vulnerable to a disorder can be pinpointed, this anatomical information can guide a search for the disorder’s root cause. Accordingly, Dr. Small’s ‘anatomical biology’ lab has pioneered the development of MRI tools best suited to isolate vulnerable hippocampal regions. His lab has then used this information to identify mechanisms that are now thought to underlie Alzheimer’s disease, schizophrenia, and ‘cognitive aging’. Most recently, his lab has begun developing interventions for each condition. To date, the lab has completed two clinical trials for cognitive aging and one for schizophrenia, and the lab’s Alzheimer’s disease findings was the cornerstone around which a new biotechnology company, Retromer Therapeutics. was formed. |
|---|
| 10:00 - 10:20 |
Deciphering the role of the LRRK2-Rab signalling pathway in Parkinson’s disease
Autosomal dominant missense mutations that hyperactivate the LRRK2 protein kinase are a common cause of inherited Parkinson’s disease and therapeutic efficacy of LRRK2 inhibitors is being tested in clinical trials. Alessi will give an overview of the nuts and bolts of current research that has revealed that LRRK2 phosphorylates a subset of Rab GTPases within their Switch-II motif controlling interaction with a new set of effectors such as RILPL1/2 and JIP3/JIP4. He will discuss what is known about how LRRK2 regulates ciliogenesis, the endosomal-lysosome system, and immune responses and how this might be linked to Parkinson’s disease. He will consider how mutations in other components linked to Parkinson’s such as Rab29 and VPS35 promote LRRK2 mediated Rab protein phosphorylation. He will discuss the identification and characterisation of a novel PPM family phosphatase member that counteracts LRRK2 signalling by dephosphorylating Rab proteins. Alessi will present data that indicates that the LRRK2 parlog termed LRRK1 also functions as a Rab kinase. 
Professor Dario Alessi FRS, University of Dundee, UK

Professor Dario Alessi FRS, University of Dundee, UKDario is biochemist whose research focuses on unravelling the roles of poorly characterised components which regulate protein phosphorylation or ubiquitylation pathways linked to human disease. He has contributed to our understanding of several disease relevant signal transduction pathways including PDK1 (diabetes and cancer), LKB1 (cancer), WNKs (blood pressure). Much of Dario’s current work is focused on understanding LRRK2 and how mutations in this enzyme cause Parkinson’s disease. In 1997 Dario became a program leader in the MRC Protein Phosphorylation and Ubiquitylation Unit, where he was appointed as its Director in 2012. He also serves as the Director of the Dundee Signal Transduction Therapy Unit, that is a collaboration between scientists at the University of Dundee and pharmaceutical companies. Dario is passionate about the role that biochemical analysis can play in opening up our understanding of human health and disease. Dario Alessi’s publications have accumulated over 9,0000 citations (h-index 145). He has obtained several awards including the Francis Crick Medal and Lecture (2006) and election to the UK Royal Society (2008). Dario obtained a BSc (1988) and PhD (1991) from the University of Birmingham and carried out postdoctoral at the University of Dundee from (1991 to 1996). |
|---|---|
| 10:20 - 10:40 |
Unravelling immune system defects downstream of endolysosomal dysfunction in a Drosophila model of Parkinson’s disease
Bi-allelic mutations have been known for many years to cause Gaucher disease (GD), the commonest lysosomal storage disorder. More recently a strong link between GBA1 loss-of-function mutations and Parkinson’s disease (PD) has been established. Numerous large multicentre genetic studies have confirmed that heterozygous GBA1 mutations are the greatest genetic risk factor for PD, conferring a ~20-fold increased risk. We have previously developed a Drosophila model of GBA1 knockout using homologous recombination. Flies lacking GBA1 display reduced survival, locomotor abnormalities and hypersensitivity to oxidative stress. They also exhibit elevated levels of the substrate glucosylceramide and lysosomal-autophagic dysfunction, with an increase in size and number of lysosomes as well as elevated autophagy substrates in the brain. The lysosomal-autophagic abnormalities occur in association with mitochondrial pathology, synaptic loss and neurodegeneration, recapitulating the main cellular features of neuronopathic GD. Thus, the GBA1 knockout fly model is well-placed to unravel the pathologies downstream of the lysosomal-autophagic dysfunction seen in GBA1-linked PD and GD. Genetic studies have revealed gene enrichment for innate immune system genes in the brains of GBA1 knockout flies. Indeed, there is increasing clinical and experimental evidence linking immune system dysfunction to PD, with elevated levels of proinflammatory cytokines both in the serum and cerebrospinal fluid of PD patients. Here Dr Kinghorn discusses the insights we have gained from studying the immune system of GBA1 knockout flies and address how immune dysfunction is likely modulating gut-brain cross-talk in GBA1-linked PD and GD. 
Dr Kerri Kinghorn, University College London, UK

Dr Kerri Kinghorn, University College London, UKDr Kerri Kinghorn is a Wellcome Trust Clinical Research Career Development Fellow at the Institute of Healthy Ageing, University College London (UCL) and an Honorary Consultant Neurologist at the National Hospital for Neurology and Neurosurgery. She completed the MB/PhD programme at the University of Cambridge and post-doctoral research at UCL as a Wellcome Clinical Fellow. This was followed by an Academic Clinical Lecturer post in neurology at Kings College London and a Rosetrees UCL Excellence Fellowship. Dr Kinghorn's research group seeks to understand the underlying pathogenic mechanisms of neurodegenerative disorders using the fruit fly Drosophila melanogaster, as well as cellular models of disease. Her research is focused on unravelling the underlying mechanisms linking genes involved in endosomal-lysosomal intracellular trafficking pathways and Parkinson’s disease. Her current works seeks to understand how endo-lysosomal autophagic defects in the gut and associated changes in its microbiome influence brain pathology via gut-brain axis communication.
|
| 10:40 - 11:00 |
Activation of the Parkinson’s associated kinase LRRK2 at lysosomal membranes
Gain of function mutations in the LRRK2 gene that encodes Leucine-rich repeat kinase 2 cause autosomal dominant Parkinson’s disease (PD). Additionally, non-coding variation at the LRRK2 locus contributes to genetic risk of sporadic PD. Prior data has strongly implicated LRRK2 in intracellular membrane trafficking by virtue of localisation to multiple cellular membranes and by phosphorylation of membrane associated Rab proteins. Furthermore, a prominent feature of LRRK2 knockout mice is the accumulation of swollen and enlarged lysosomes, suggesting that the endogenous LRRK2 protein regulates some aspect of lysosomal trafficking. The group has recently shown that lysosomal damage induced by exposure of cultured cells to L-leucyl-L-leucine methyl ester (LLOMe) causes recruitment of LRRK2 to the lysosomal membrane and activation of kinase activity. This results in the phosphorylation of lysosomal Rab proteins that then interact with the cytoskeletal adaptor protein JIP4 and leads to tubulation of the lysosomal membrane to form vesicles that can migrate to undamaged lysosomes in the same cell. The group has named this process LYTL (lysosomal tubulation induced by LRRK2) and further show that (1) coding mutant forms of LRRK2 enhance LYTL leading to excessive tubulation in cultured astrocytes and that (2) non-coding variation in the 5’ region of the LRRK2 gene also enhances LRRK2 activation in response to LLOMe in IPSC-derived microglial cells. These results imply that multiple types of genetic variation around LRRK2 share the same direction of effect and, by extension, suggest that inhibiting LRRK2 may be a novel therapeutic approach for both inherited and sporadic PD. 
Dr Mark Cookson, NIA, NIH, USA

Dr Mark Cookson, NIA, NIH, USADr Mark R Cookson is a cell biologist whose current research interests include the effects of mutations in the genes associated with neurodegeneration at the cellular and molecular level. His laboratory efforts are directed at finding the underlying pathways that lead to Parkinson's disease and related disorders. Dr Cookson received both his BSc and PhD degrees from the University of Salford, UK in 1991 and 1995, respectively. His postdoctoral studies included time spent at the Medical Research Council laboratories and at the University of Newcastle, UK. He joined the Mayo Clinic, Jacksonville, Florida, as an Assistant Professor in 2000 and moved to the NIA in February 2002. Within the Laboratory of Neurogenetics, Dr Cookson's group works on the effects of mutations associated with Parkinson's disease on protein function. |
| 11:00 - 11:20 |
Endo-lysosomal dysfunction – a unifying mechanism for hereditary spastic paraplegia
Hereditary spastic paraplegias are genetic conditions in which corticospinal tract axons selectively generate. Mutations in the microtubule severing ATPase spastin are the most common cause of the condition. In this talk Dr Reid will describe his work in studying the role of spastin at endosomes and how abnormality of this translates to lysosomal dysfunction in axons. He will demonstrate that spastin is required for efficient endosomal tubule fission at the point of contacts between endosomal tubules and the endoplasmic reticulum. Defective endosomal tubule fission in cells lacking spastin has consequences for receptor sorting away from the endosomal pathway; notably it causes a block in endosome-to-Golgi mannose 6-phosphate receptor (M6PR) traffic. The normal function of M6PR is to collect lysosomal enzymes from the Golgi and traffic them back to the endolysosomal compartment, so lack of M6PR at the Golgi in cells lacking spastin is associated with abnormal lysosomal enzyme traffic and defects in lysosomal morphology and function. In neurons from a spastin-HSP knock-in mouse model and in human neurons derived reprogrammed from spastin patient fibroblasts, abnormal lysosomes are found within pathological axonal swellings, potentially explaining the axonopathy in spastin-HSP. Work will also be presented that indicates that lysosomal dysfunction is a unifying pathological mechanism across many different HSP genetic subtypes. 
Dr Evan Reid, Cambridge Institute of Medical Research, UK

Dr Evan Reid, Cambridge Institute of Medical Research, UKEvan Reid graduated in Medicine from Glasgow University in 1991 then trained in Medical Genetics in Glasgow and Cambridge. He became interested in the hereditary spastic paraplegias (HSPs), which are genetic forms of motor neuron degeneration. He completed a PhD in Cambridge studying the genetics of these conditions, supervised by David Rubinsztein. After stints as a Wellcome Trust Advanced and then Senior Research Fellow, he is now Reader in Neurogenetics and Molecular Neurobiology and Principal Investigator at the Cambridge Institute for Medical Research, a research institute of the University of Cambridge that has a strategic focus on unravelling the mechanisms of rare genetic disease. He is clinically active and runs a specialised neurogenetics clinic at Addenbrooke's Hospital. His research has encompassed the clinical features, genetics and cell biology of HSPs, but concentrates on understanding the molecular pathology of HSP proteins that are involved in membrane traffic. |
| 11:20 - 11:40 |
Hyperactive LRRK2 kinase alters neuronal autophagy by disrupting the axonal transport of autophagosomes
Neurons rely on autophagy, a critical homeostatic mechanism, to maintain cellular health over the decades of human life. Deficits in autophagy cause the accumulation of protein aggregates and dysfunctional mitochondria, and are characteristic of major neurodegenerative diseases including Parkinson’s disease (PD). The group has identified a constitutive and nonselective pathway for axonal autophagy, in which autophagosomes are generated preferentially in the distal axon and then rapidly transported to the soma by molecular motors interacting with the microtubule cytoskeleton. Here, the group asked how this pathway is altered in neurons expressing the most common PD-causing mutation in LRRK2; the G2019S mutation induces hyperactive LRRK2 kinase activity leading to increased phosphorylation of Rab GTPases that regulate intracellular trafficking. They found that LRRK2-G2019S significantly reduces the processivity of autophagosome transport along axons. Similar effects were observed across multiple models, including hippocampal neurons overexpressing mutant LRRK2, cortical neurons from a knock-in mouse, and human iPSC-derived neurons gene-edited to express the G2019S mutation. Altered transport led to impaired organelle maturation; this deficit was reversed by pharmacological inhibition of LRRK2 kinase activity. The group probed the underlying mechanism, and found that hyperactive LRRK2 recruits the motor adaptor JIP4 to the autophagosomal membrane, inducing abnormal activation of kinesin and resulting in a tug-of-war between anterograde and retrograde motors bound to the organelle and thus inhibition of processive unidirectional motility. Together, these findings demonstrate that increased LRRK2 kinase activity is sufficient to induce defects in autophagosome transport and maturation, further implicating defective autophagy in the pathogenesis of Parkinson’s disease. 
Professor Erika Holzbaur, University of Pennsylvania, USA

Professor Erika Holzbaur, University of Pennsylvania, USAErika Holzbaur is the William Maul Measey Professor of Physiology at the University of Pennsylvania Perelman School of Medicine. She received her BS in Chemistry and History from the College of William and Mary, her PhD in Biochemistry from Penn State, and performed her postdoctoral studies at the Worcester Foundation for Experimental Biology. Dr Holzbaur was recruited to Penn in 1992 and now holds an endowed chair. The Holzbaur lab studies the dynamics of organelle motility along the cellular cytoskeleton, required to drive the active transport of organelles along the axons and dendrites of neurons. The lab also investigates cellular mechanisms leading to neurodegeneration focusing on autophagy and mitophagy, pathways critical to maintain neuronal homeostasis. Dr Holzbaur was appointed a Porter Fellow and has received the NINDS Javits Award, the Stanley N. Cohen Biomedical Research Award, and is an inaugural Lifetime Fellow of the American Society for Cell Biology. |
| 11:40 - 11:50 |
Selected short presentation
Autophagosomal maturity coordinates dynein effector scaffolding in axons Sydney E Cason, Peter Carman, Claire Van Duyne, Roberto Dominguez, and Erika LF Holzbaur Autophagy is a degradative pathway required to maintain neuronal homeostasis. Neuronal autophagosomes form at the axon terminal and mature via lysosomal fusion during dynein-mediated transport to the soma. How the dynein-autophagosome interaction is regulated during this maturation is unknown. This research reveals a series of handoffs between dynein effectors as autophagosomes transit along the axons of primary neurons. Autophagosomes in the distal axon require JIP1 to initiate transport, while autophagosomes in the mid-axon require HAP1 and Huntingtin for motility. HAP1 is a bonafide dynein activator and binds the dynein-dynactin complex via canonical and noncanonical interactions. Lysosomal protein JIP3 associates with most axonal autophagic vacuoles but specifically regulates the transport of autolysosomes. Inhibiting autophagosomal transport disrupts maturation, and this work finds that inhibiting autophagosomal maturation perturbs the association and function of autophagosomal dynein effectors. Thus maturation state and transport are tightly linked. Collectively, these results describe a novel maturation-based motor effector handoff on neuronal autophagosomes key to autophagosomal motility, degradation, and ultimately axonal health. Supported by NIH grant R35 GM126950. |
| 11:50 - 12:00 |
Selected short presentation
A role for adaptor protein complex 4 in the spatial control of endocannabinoid synthesis Alexandra K Davies1, Giovanni Cardone1, Catherine G Vasilopoulou1, Marvin Ziegler2, Hellen Jumo2, Wardiya Afshar Saber2, Darius Ebrahimi-Fakhari2 and Georg HH Borner1 1Max Planck Institute of Biochemistry, Germany The localisation of diacylglycerol (DAG) lipases determines sites of synthesis of 2-AG, the most abundant endocannabinoid in brain. DAG lipases are targeted to growing axons where 2-AG is required to promote axonal growth by activation of cannabinoid receptors. However, the machinery for axonal transport of DAG lipases is currently unknown. The recently characterised adaptor protein complex 4 (AP-4) transport pathway mediates delivery of trans-Golgi network (TGN)-derived vesicles to the axon. Patients with AP-4 deficiency syndrome have a severe neurological disorder with axonal degeneration leading to spasticity and intellectual disability. Here, spatial proteomics data from AP-4-deficient HeLa cells revealed that DAG lipase-beta (DAGLB) is a cargo of AP-4. In several AP-4 deficient cell types, including iPSC-derived neurons from an AP-4 patient, DAGLB accumulates at the TGN. Furthermore, DAGLB co-localises with AP-4 vesicle proteins, in an AP-4 dependent manner, and overexpression of the AP-4 motor adaptor RUSC2 drives DAGLB-containing vesicles to the plus-ends of microtubules. These data strongly support that AP-4-mediated transport is responsible for the axonal targeting of DAGLB. This model provides a missing link in the regulation of endocannabinoid signalling in neurons and suggests that aberrant spatial control of 2-AG synthesis may contribute to axonal defects in AP-4 deficiency syndrome. |
Chair

Professor Selina Wray, UCL, UK

Professor Selina Wray, UCL, UK
Selina Wray is a Professor of Molecular Neuroscience and Alzheimer's Research UK Senior Research Fellow in the Department of Neurodegenerative Disease at UCL Queen Square Institute of Neurology. Selina was awarded her PhD in 2009 from Kings College London, prior to moving to UCL Queen Square Institute of Neurology as an Alzheimer's Research UK Junior research fellow in the group of Professor John Hardy. Selina’s work is focused on the use of induced pluripotent stem cell (iPSC) technology to model dementia, working closely with clinical colleagues to obtain samples from participants with rare, genetic forms of dementia and using these to understand the molecular basis of Alzheimer's Disease and Frontotemporal Dementia.

Dr Guillaume van Niel, Université de Paris, IPNP, INSERM, GHU Hopital Saint Anne, Paris, France

Dr Guillaume van Niel, Université de Paris, IPNP, INSERM, GHU Hopital Saint Anne, Paris, France
Guillaume van Niel is research director leading the team 'endosomal dynamic in neuropathies' at the Institute of Psychiatry and Neurosciences of Paris (IPNP). G van Niel contributed for 20 years to the understanding of the biogenesis and function of exosomes and mutlivesicular endosomes from various cell types, in particular in antigen presentation and in physiological amyloid formation. His recent work has used cutting edge imaging methods to investigate exosome biogenesis and fate in vitro and in vivo. His current fundamental research projects aim at better understanding the dynamic of the endolysosomal system and exosomes in neuropathies such Alzheimer’s Disease and glioblastoma development using zebrafish as model organism. In parallel he is setting up an in vivo screening platform to establish the zebrafish as a relevant preclinical model organism for applied EV research.
| 13:00 - 15:00 |
Live panel discussion

Professor Dario Alessi FRS, University of Dundee, UK

Professor Dario Alessi FRS, University of Dundee, UKDario is biochemist whose research focuses on unravelling the roles of poorly characterised components which regulate protein phosphorylation or ubiquitylation pathways linked to human disease. He has contributed to our understanding of several disease relevant signal transduction pathways including PDK1 (diabetes and cancer), LKB1 (cancer), WNKs (blood pressure). Much of Dario’s current work is focused on understanding LRRK2 and how mutations in this enzyme cause Parkinson’s disease. In 1997 Dario became a program leader in the MRC Protein Phosphorylation and Ubiquitylation Unit, where he was appointed as its Director in 2012. He also serves as the Director of the Dundee Signal Transduction Therapy Unit, that is a collaboration between scientists at the University of Dundee and pharmaceutical companies. Dario is passionate about the role that biochemical analysis can play in opening up our understanding of human health and disease. Dario Alessi’s publications have accumulated over 9,0000 citations (h-index 145). He has obtained several awards including the Francis Crick Medal and Lecture (2006) and election to the UK Royal Society (2008). Dario obtained a BSc (1988) and PhD (1991) from the University of Birmingham and carried out postdoctoral at the University of Dundee from (1991 to 1996). 
Dr Kerri Kinghorn, University College London, UK

Dr Kerri Kinghorn, University College London, UKDr Kerri Kinghorn is a Wellcome Trust Clinical Research Career Development Fellow at the Institute of Healthy Ageing, University College London (UCL) and an Honorary Consultant Neurologist at the National Hospital for Neurology and Neurosurgery. She completed the MB/PhD programme at the University of Cambridge and post-doctoral research at UCL as a Wellcome Clinical Fellow. This was followed by an Academic Clinical Lecturer post in neurology at Kings College London and a Rosetrees UCL Excellence Fellowship. Dr Kinghorn's research group seeks to understand the underlying pathogenic mechanisms of neurodegenerative disorders using the fruit fly Drosophila melanogaster, as well as cellular models of disease. Her research is focused on unravelling the underlying mechanisms linking genes involved in endosomal-lysosomal intracellular trafficking pathways and Parkinson’s disease. Her current works seeks to understand how endo-lysosomal autophagic defects in the gut and associated changes in its microbiome influence brain pathology via gut-brain axis communication.

Dr Evan Reid, Cambridge Institute of Medical Research, UK

Dr Evan Reid, Cambridge Institute of Medical Research, UKEvan Reid graduated in Medicine from Glasgow University in 1991 then trained in Medical Genetics in Glasgow and Cambridge. He became interested in the hereditary spastic paraplegias (HSPs), which are genetic forms of motor neuron degeneration. He completed a PhD in Cambridge studying the genetics of these conditions, supervised by David Rubinsztein. After stints as a Wellcome Trust Advanced and then Senior Research Fellow, he is now Reader in Neurogenetics and Molecular Neurobiology and Principal Investigator at the Cambridge Institute for Medical Research, a research institute of the University of Cambridge that has a strategic focus on unravelling the mechanisms of rare genetic disease. He is clinically active and runs a specialised neurogenetics clinic at Addenbrooke's Hospital. His research has encompassed the clinical features, genetics and cell biology of HSPs, but concentrates on understanding the molecular pathology of HSP proteins that are involved in membrane traffic. 
Dr Mark Cookson, NIA, NIH, USA

Dr Mark Cookson, NIA, NIH, USADr Mark R Cookson is a cell biologist whose current research interests include the effects of mutations in the genes associated with neurodegeneration at the cellular and molecular level. His laboratory efforts are directed at finding the underlying pathways that lead to Parkinson's disease and related disorders. Dr Cookson received both his BSc and PhD degrees from the University of Salford, UK in 1991 and 1995, respectively. His postdoctoral studies included time spent at the Medical Research Council laboratories and at the University of Newcastle, UK. He joined the Mayo Clinic, Jacksonville, Florida, as an Assistant Professor in 2000 and moved to the NIA in February 2002. Within the Laboratory of Neurogenetics, Dr Cookson's group works on the effects of mutations associated with Parkinson's disease on protein function. 
Professor Erika Holzbaur, University of Pennsylvania, USA

Professor Erika Holzbaur, University of Pennsylvania, USAErika Holzbaur is the William Maul Measey Professor of Physiology at the University of Pennsylvania Perelman School of Medicine. She received her BS in Chemistry and History from the College of William and Mary, her PhD in Biochemistry from Penn State, and performed her postdoctoral studies at the Worcester Foundation for Experimental Biology. Dr Holzbaur was recruited to Penn in 1992 and now holds an endowed chair. The Holzbaur lab studies the dynamics of organelle motility along the cellular cytoskeleton, required to drive the active transport of organelles along the axons and dendrites of neurons. The lab also investigates cellular mechanisms leading to neurodegeneration focusing on autophagy and mitophagy, pathways critical to maintain neuronal homeostasis. Dr Holzbaur was appointed a Porter Fellow and has received the NINDS Javits Award, the Stanley N. Cohen Biomedical Research Award, and is an inaugural Lifetime Fellow of the American Society for Cell Biology. |
|---|
| 16:00 - 17:00 |
Early career 'table' discussions

Professor Dario Alessi FRS, University of Dundee, UK

Professor Dario Alessi FRS, University of Dundee, UKDario is biochemist whose research focuses on unravelling the roles of poorly characterised components which regulate protein phosphorylation or ubiquitylation pathways linked to human disease. He has contributed to our understanding of several disease relevant signal transduction pathways including PDK1 (diabetes and cancer), LKB1 (cancer), WNKs (blood pressure). Much of Dario’s current work is focused on understanding LRRK2 and how mutations in this enzyme cause Parkinson’s disease. In 1997 Dario became a program leader in the MRC Protein Phosphorylation and Ubiquitylation Unit, where he was appointed as its Director in 2012. He also serves as the Director of the Dundee Signal Transduction Therapy Unit, that is a collaboration between scientists at the University of Dundee and pharmaceutical companies. Dario is passionate about the role that biochemical analysis can play in opening up our understanding of human health and disease. Dario Alessi’s publications have accumulated over 9,0000 citations (h-index 145). He has obtained several awards including the Francis Crick Medal and Lecture (2006) and election to the UK Royal Society (2008). Dario obtained a BSc (1988) and PhD (1991) from the University of Birmingham and carried out postdoctoral at the University of Dundee from (1991 to 1996). 
Dr Kerri Kinghorn, University College London, UK

Dr Kerri Kinghorn, University College London, UKDr Kerri Kinghorn is a Wellcome Trust Clinical Research Career Development Fellow at the Institute of Healthy Ageing, University College London (UCL) and an Honorary Consultant Neurologist at the National Hospital for Neurology and Neurosurgery. She completed the MB/PhD programme at the University of Cambridge and post-doctoral research at UCL as a Wellcome Clinical Fellow. This was followed by an Academic Clinical Lecturer post in neurology at Kings College London and a Rosetrees UCL Excellence Fellowship. Dr Kinghorn's research group seeks to understand the underlying pathogenic mechanisms of neurodegenerative disorders using the fruit fly Drosophila melanogaster, as well as cellular models of disease. Her research is focused on unravelling the underlying mechanisms linking genes involved in endosomal-lysosomal intracellular trafficking pathways and Parkinson’s disease. Her current works seeks to understand how endo-lysosomal autophagic defects in the gut and associated changes in its microbiome influence brain pathology via gut-brain axis communication.

Dr Evan Reid, Cambridge Institute of Medical Research, UK

Dr Evan Reid, Cambridge Institute of Medical Research, UKEvan Reid graduated in Medicine from Glasgow University in 1991 then trained in Medical Genetics in Glasgow and Cambridge. He became interested in the hereditary spastic paraplegias (HSPs), which are genetic forms of motor neuron degeneration. He completed a PhD in Cambridge studying the genetics of these conditions, supervised by David Rubinsztein. After stints as a Wellcome Trust Advanced and then Senior Research Fellow, he is now Reader in Neurogenetics and Molecular Neurobiology and Principal Investigator at the Cambridge Institute for Medical Research, a research institute of the University of Cambridge that has a strategic focus on unravelling the mechanisms of rare genetic disease. He is clinically active and runs a specialised neurogenetics clinic at Addenbrooke's Hospital. His research has encompassed the clinical features, genetics and cell biology of HSPs, but concentrates on understanding the molecular pathology of HSP proteins that are involved in membrane traffic. 
Dr Mark Cookson, NIA, NIH, USA

Dr Mark Cookson, NIA, NIH, USADr Mark R Cookson is a cell biologist whose current research interests include the effects of mutations in the genes associated with neurodegeneration at the cellular and molecular level. His laboratory efforts are directed at finding the underlying pathways that lead to Parkinson's disease and related disorders. Dr Cookson received both his BSc and PhD degrees from the University of Salford, UK in 1991 and 1995, respectively. His postdoctoral studies included time spent at the Medical Research Council laboratories and at the University of Newcastle, UK. He joined the Mayo Clinic, Jacksonville, Florida, as an Assistant Professor in 2000 and moved to the NIA in February 2002. Within the Laboratory of Neurogenetics, Dr Cookson's group works on the effects of mutations associated with Parkinson's disease on protein function. 
Professor Erika Holzbaur, University of Pennsylvania, USA

Professor Erika Holzbaur, University of Pennsylvania, USAErika Holzbaur is the William Maul Measey Professor of Physiology at the University of Pennsylvania Perelman School of Medicine. She received her BS in Chemistry and History from the College of William and Mary, her PhD in Biochemistry from Penn State, and performed her postdoctoral studies at the Worcester Foundation for Experimental Biology. Dr Holzbaur was recruited to Penn in 1992 and now holds an endowed chair. The Holzbaur lab studies the dynamics of organelle motility along the cellular cytoskeleton, required to drive the active transport of organelles along the axons and dendrites of neurons. The lab also investigates cellular mechanisms leading to neurodegeneration focusing on autophagy and mitophagy, pathways critical to maintain neuronal homeostasis. Dr Holzbaur was appointed a Porter Fellow and has received the NINDS Javits Award, the Stanley N. Cohen Biomedical Research Award, and is an inaugural Lifetime Fellow of the American Society for Cell Biology. |
|---|
| 10:00 - 10:20 |
Protein truncating variants in the SORL1 gene are associated with >35-fold increased risk and earlier onset of Alzheimer's disease
Rare protein truncating or missense variants in the SORL1 gene are associated with an increased risk and possibly a causative effect on developing Alzheimer’s Disease (AD). Here, the group investigated the relationship between the predicted variant pathogenicity, variant frequency, the age at AD onset (aao) and increased AD-risk in the largest whole exome sequencing (WES) dataset of AD cases and controls world-wide. In sequencing data from 12,675 AD cases and 8,693 controls from the ADES and ADSP consortia the group identified 470 missense or LOF SORL1 variants with allele frequencies <1% in the sample. Damagingness of missense variants was scored using the REVEL algorithm and damagingness of loss of function (LOF) variants was scored using the CADD algorithm; CADD score >30 is considered pathogenic. These results open the discussion of whether carriers of a LOF SORL1-variant and their (presymptomatic) family-members should be clinically counselled. For this, pathogenicity screens that distinguish between pathogenic and non-pathogenic non-synonymous variants are warranted. Furthermore, the profound effects of LOF and damaging nonsynonymous variants on AD risk makes the SORL1 protein product a promising target for the design of selective treatment strategies for individuals affected with SORL1-associated AD. 
Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The Netherlands

Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The NetherlandsHenne Holstege is an Associate Professor at the Amsterdam University Medical Center. After she majored in biochemistry at the University of Leiden she did her PhD at the Netherlands Cancer Institute. During this time Dr Holstege was intrigued by the extraordinary case of a Dutch woman who died at age 115 without any symptoms of cognitive decline because this woman proved that cognitive decline is not inevitable. Holstege set up the 100-plus Study, a cohort study of cognitively healthy centenarians to identify protective genetic and biomolecular factors that associate with the escape of cognitive decline. She analyses the data from the centenarians in context of the genetics and biomolecular factors of (early onset) Alzheimer’s Disease; both extremes on the same cognitive spectrum. Therefore, her lab is involved in large international collaborative joint analysis of sequencing data thousands of Alzheimer Disease cases and cognitively healthy controls the collected by European ADES and American ADSP consortia. Holstege and collaborators are currently identifying novel genes associated with the increased or decreased risk of AD. Here, she applies specific focus on the identification of rare pathogenic variants in the SORL1 gene, which next to APOE-e4 allele, is the most common and strongest risk factor of AD. One of her major goals is, therefore, is to implement adequate clinical counselling strategies of SORL1 variant to the carriers and their family members. For this reason, a part of her lab is embedded in the clinic, and involved in counseling genetically predisposed Alzheimer Disease patients. For her work, Holstege was awarded the Alzheimer Research Prize by the Hans und Ilse Breuer Foundation in 2020. For more information see: www.holstegelab.eu. |
|---|---|
| 10:20 - 10:40 |
Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, Canada

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, Canada

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, CanadaPeter St George-Hyslop FRS is a medical scientist, neurologist and molecular geneticist who is distinguished for his research into neurodegenerative disorders, including Alzheimer’s disease (AD). In particular, he discovered several genes that when mutated lead to early onset hereditary AD, accelerating our understanding the disease and the development of potential treatments. His discovery that defective genes encoding presenilins are a cause of familial AD led to presenilins becoming a new target for treatments. He went on to show that mutated presenilins contribute to the generation of the amyloid beta protein — deposition of which is the earliest sign of AD in those carrying such genes. His work on several other neurodegeneration-related genes and proteins (including SORLA, TREM2, FUS and ANXA11) has led to an understanding of the role of vesicular transport, inflammation and perturbed RNA granule biology. Peter has led an AD research programme as Professor of Experimental Neuroscience at the University of Cambridge since 2007. He was awarded the Howard Hughes Medical Institute International Scholar Award in both 1997 and 2002, and has received several other notable awards. |
| 10:40 - 11:00 |
Rescuing autophagosome and lysosome defects in C9ORF72 ALS/FTD by inhibiting PIKFYVE kinase
An intronic GGGGCC repeat expansion in C9ORF72 is the most common cause of amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD), but the pathogenic mechanism of this repeat remains unclear. Using human induced motor neurons (iMNs), the group found that repeat-expanded C9ORF72 was haploinsufficient in ALS. They found that C9ORF72 interacted with endosomes and was required for normal vesicle trafficking and lysosomal biogenesis in motor neurons. Repeat expansion reduced C9ORF72 expression, triggering neurodegeneration through two mechanisms: accumulation of glutamate receptors, leading to excitotoxicity, and impaired clearance of neurotoxic dipeptide repeat proteins derived from the repeat expansion. Thus, cooperativity between gain- and loss-of-function mechanisms led to neurodegeneration. Restoring C9ORF72 levels, augmenting its function with constitutively active RAB5, or compensating for its loss by inhibiting PIKFYVE and activating secretory autophagy ameliorated neurodegenerative processes in both gain- and loss-of-function C9ORF72 mouse models. Thus, modulating vesicle trafficking was able to rescue neurodegeneration caused by the C9ORF72 repeat expansion. Coupled with rare mutations in ALS2, FIG4, CHMP2B, OPTN and SQSTM1, these results reveal mechanistic convergence on vesicle trafficking in ALS and FTD. 
Dr Justin Ichida, University of Southern California, USA

Dr Justin Ichida, University of Southern California, USAJustin K Ichida is an Associate Professor of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC. Prior to joining USC, Dr Ichida earned his PhD at Harvard Medical School studying the origins of life with Jack Szostak and did postdoctoral work on cellular reprogramming with Kevin Eggan at Harvard University. Dr Ichida conducts research on the etiology, pathogenesis, genetics, and treatment of neurodegenerative diseases, with a focus on amyotrophic lateral sclerosis (ALS) and frontotemporal dementia. His work has garnered many awards, including a Pathway to Independence Award from the National Institutes of Health, the New York Stem Cell Foundation Innovator Award, the Richard N. Merkin Scholar Award, and the Donald and Delia Baxter Foundation Faculty Scholar Award. In December 2017, Ichida received the Champion for a Cure Award from the ALS Association, the highest honor the ALS Association bestows on scientists for distinguished intellectual achievements. Since starting at USC in 2013, Dr Ichida has secured more than $15 million in external funding for research on ALS, frontotemporal dementia, Alzheimer’s disease, and other disorders of the nervous system. Ichida has published 68 scientific papers in the scientific literature and has co-founded a Los Angeles-based biotech company to translate findings from his lab to the clinic. |
| 11:00 - 11:20 |
Therapeutic effects of retromer stabilization in Amyotrophic Lateral Sclerosis models
Amyotrophic Lateral Sclerosis (ALS) is a fatal disease characterised by the degeneration of upper and lower motor neurons (MNs). Protein aggregation and misfolding likely contribute to MNs cell death, and therefore their clearance may represent a therapeutic strategy with the potential to enter the clinical practice. The retromer is a multi-protein complex involved in retrograde transport of proteins from endosomes to the trans-Golgi network and to the cell membrane. The group found significantly reduced levels of the retromer complex subunit VPS35 in iPSCs-derived MNs from ALS patients, in MNs from ALS post mortem explants and in MNs from SOD1G93A mice. Being the retromer involved in trafficking of hydrolases – a pathological hallmark in ALS – they rationally designed and synthesized an array of retromer stabilisers based on bis-guanylhydrazones connected by a 1,3-phenyl ring linker. Such molecules, working as a pharmacological chaperone, increased the stability/functioning of retromer in vitro and in vivo. Among them, the group selected leading compound 2a as a potent and bioavailable interactor of VPS35-VPS29. Indeed, while increasing retromer stability in ALS mice, compound 2a attenuated locomotion impairment and increased MNs survival. Moreover, compound 2a increased VPS35 in iPSCs-derived MNs and showed a high brain bioavailability. These results clearly suggest the retromer as a valuable 'druggable' target in ALS. 
Professor Pierfausto Seneci, University of Milan, Italy

Professor Pierfausto Seneci, University of Milan, ItalyPierfausto Seneci received his degree in Chemistry in Pavia, followed by a postdoc at Politecnico (Milan). From 1986 he worked at Pierrel (Milan) on heterocyclic NSAIDs; at Marion Merrell Dow, on semisynthetic modification of natural antibacterials (Gerenzano), and on neuroprotective agents (Strasbourg); at Selectide (Tucson, USA) on combinatorial libraries of natural product-like structures; at SmithKlineBeecham (Rennes) as Lab Head of Chemistry, working in oncology and osteoporosis; and at GlaxoWellcome (Verona) as Director of Lead Discovery, leading the optimization of antibacterial and CNS agents. In 2000 he was a co-founder and CSO of NADAG (Munich), working on disease-modifying agents to cure AD. In 2003 he became Associate Professor at the University of Milan, where he teaches basic and advanced courses. His medicinal chemistry interests are in oncology (pro-apoptotics, natural product derivatives, immuno-oncology) and in neurodegeneration (disease-modifyers against AD, PD and ALS). He authored more than 120 papers, 15 patents and 4 books. 
Dr Luca Muzio, San Raffaele Scientific Institute, Italy

Dr Luca Muzio, San Raffaele Scientific Institute, ItalyLuca Muzio received his degree in Biology in Genoa. He is a senior scientist at the Institute of Experimental Neurology (INSpe) of San Raffaele Scientific Institute, Italy. He is a trained biologist that completed his PhD in 2005, working in the field of developmental biology. It is in that context that he investigated transcription factors and molecular mechanisms involved in cortical development. In 2006, he joined the INSpe and he has made research contributions in the field of neuroimmunology. He carried out different types of experiments and researches on animal models of multiple sclerosis (MS). More recently, he started to investigate neurodegeneration in Amyotrophic Lateral Sclerosis (ALS). He did researches focused on microglia activation in ALS models and recently he started to investigate the retromer molecular pathway. Starting from 2015, he teaches at the University Vita Salute of Milan. |
| 11:20 - 11:30 |
Selected short presentation
sCJD GWAS: identification, replication and functional validation of risk at STX6 locus Emma Jones, Holger Hummerich, James Uphill, Christian Schmidt, Parvin Ahmed, John Collinge, Emmanuelle Viré, Simon Mead Sporadic Creutzfeldt-Jakob disease (sCJD) is the most common human prion disease, caused by the apparent spontaneous misfolding of cellular prion protein into disease-associated assemblies. Although there is clear genetic control in sCJD, no loci except PRNP have been identified as consistently significant. The current project utilised a two-stage genome wide association study (GWAS) design comprising 5,208 sCJD cases and 511,585 matched controls obtained through international collaboration. This resulted in the first replicated association of two novel loci alongside PRNP, with variants in or near STX6 and GAL3ST1, as conferring risk for sCJD at genome-wide significance in populations with European ancestries. Fine-mapping and analysis of expression quantitative trait loci provides evidence for modified STX6 expression in the dorsal striatum as driving the association at this locus. Preliminary functional investigation via manipulating gene expression in N2aPK1 cells does not suggest a role of STX6 in prion replication or infectivity in this cell line. Identification of non-PRNP loci associated with sCJD risk provides new insight into disease mechanisms, including a previously unidentified role of syntaxin-6-mediated intracellular trafficking. Additionally shared genetic risk at STX6 with the tauopathy Progressive Supranuclear Palsy lends support to a common “prion-like” mechanism in related neurodegenerative diseases. |
| 13:00 - 15:00 |
Live panel discussion

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, Canada

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, CanadaPeter St George-Hyslop FRS is a medical scientist, neurologist and molecular geneticist who is distinguished for his research into neurodegenerative disorders, including Alzheimer’s disease (AD). In particular, he discovered several genes that when mutated lead to early onset hereditary AD, accelerating our understanding the disease and the development of potential treatments. His discovery that defective genes encoding presenilins are a cause of familial AD led to presenilins becoming a new target for treatments. He went on to show that mutated presenilins contribute to the generation of the amyloid beta protein — deposition of which is the earliest sign of AD in those carrying such genes. His work on several other neurodegeneration-related genes and proteins (including SORLA, TREM2, FUS and ANXA11) has led to an understanding of the role of vesicular transport, inflammation and perturbed RNA granule biology. Peter has led an AD research programme as Professor of Experimental Neuroscience at the University of Cambridge since 2007. He was awarded the Howard Hughes Medical Institute International Scholar Award in both 1997 and 2002, and has received several other notable awards. 
Dr Justin Ichida, University of Southern California, USA

Dr Justin Ichida, University of Southern California, USAJustin K Ichida is an Associate Professor of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC. Prior to joining USC, Dr Ichida earned his PhD at Harvard Medical School studying the origins of life with Jack Szostak and did postdoctoral work on cellular reprogramming with Kevin Eggan at Harvard University. Dr Ichida conducts research on the etiology, pathogenesis, genetics, and treatment of neurodegenerative diseases, with a focus on amyotrophic lateral sclerosis (ALS) and frontotemporal dementia. His work has garnered many awards, including a Pathway to Independence Award from the National Institutes of Health, the New York Stem Cell Foundation Innovator Award, the Richard N. Merkin Scholar Award, and the Donald and Delia Baxter Foundation Faculty Scholar Award. In December 2017, Ichida received the Champion for a Cure Award from the ALS Association, the highest honor the ALS Association bestows on scientists for distinguished intellectual achievements. Since starting at USC in 2013, Dr Ichida has secured more than $15 million in external funding for research on ALS, frontotemporal dementia, Alzheimer’s disease, and other disorders of the nervous system. Ichida has published 68 scientific papers in the scientific literature and has co-founded a Los Angeles-based biotech company to translate findings from his lab to the clinic. 
Professor Pierfausto Seneci, University of Milan, Italy

Professor Pierfausto Seneci, University of Milan, ItalyPierfausto Seneci received his degree in Chemistry in Pavia, followed by a postdoc at Politecnico (Milan). From 1986 he worked at Pierrel (Milan) on heterocyclic NSAIDs; at Marion Merrell Dow, on semisynthetic modification of natural antibacterials (Gerenzano), and on neuroprotective agents (Strasbourg); at Selectide (Tucson, USA) on combinatorial libraries of natural product-like structures; at SmithKlineBeecham (Rennes) as Lab Head of Chemistry, working in oncology and osteoporosis; and at GlaxoWellcome (Verona) as Director of Lead Discovery, leading the optimization of antibacterial and CNS agents. In 2000 he was a co-founder and CSO of NADAG (Munich), working on disease-modifying agents to cure AD. In 2003 he became Associate Professor at the University of Milan, where he teaches basic and advanced courses. His medicinal chemistry interests are in oncology (pro-apoptotics, natural product derivatives, immuno-oncology) and in neurodegeneration (disease-modifyers against AD, PD and ALS). He authored more than 120 papers, 15 patents and 4 books. 
Dr Luca Muzio, San Raffaele Scientific Institute, Italy

Dr Luca Muzio, San Raffaele Scientific Institute, ItalyLuca Muzio received his degree in Biology in Genoa. He is a senior scientist at the Institute of Experimental Neurology (INSpe) of San Raffaele Scientific Institute, Italy. He is a trained biologist that completed his PhD in 2005, working in the field of developmental biology. It is in that context that he investigated transcription factors and molecular mechanisms involved in cortical development. In 2006, he joined the INSpe and he has made research contributions in the field of neuroimmunology. He carried out different types of experiments and researches on animal models of multiple sclerosis (MS). More recently, he started to investigate neurodegeneration in Amyotrophic Lateral Sclerosis (ALS). He did researches focused on microglia activation in ALS models and recently he started to investigate the retromer molecular pathway. Starting from 2015, he teaches at the University Vita Salute of Milan. 
Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The Netherlands

Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The NetherlandsHenne Holstege is an Associate Professor at the Amsterdam University Medical Center. After she majored in biochemistry at the University of Leiden she did her PhD at the Netherlands Cancer Institute. During this time Dr Holstege was intrigued by the extraordinary case of a Dutch woman who died at age 115 without any symptoms of cognitive decline because this woman proved that cognitive decline is not inevitable. Holstege set up the 100-plus Study, a cohort study of cognitively healthy centenarians to identify protective genetic and biomolecular factors that associate with the escape of cognitive decline. She analyses the data from the centenarians in context of the genetics and biomolecular factors of (early onset) Alzheimer’s Disease; both extremes on the same cognitive spectrum. Therefore, her lab is involved in large international collaborative joint analysis of sequencing data thousands of Alzheimer Disease cases and cognitively healthy controls the collected by European ADES and American ADSP consortia. Holstege and collaborators are currently identifying novel genes associated with the increased or decreased risk of AD. Here, she applies specific focus on the identification of rare pathogenic variants in the SORL1 gene, which next to APOE-e4 allele, is the most common and strongest risk factor of AD. One of her major goals is, therefore, is to implement adequate clinical counselling strategies of SORL1 variant to the carriers and their family members. For this reason, a part of her lab is embedded in the clinic, and involved in counseling genetically predisposed Alzheimer Disease patients. For her work, Holstege was awarded the Alzheimer Research Prize by the Hans und Ilse Breuer Foundation in 2020. For more information see: www.holstegelab.eu. |
|---|
Chair

Professor Pierfausto Seneci, University of Milan, Italy

Professor Pierfausto Seneci, University of Milan, Italy
Pierfausto Seneci received his degree in Chemistry in Pavia, followed by a postdoc at Politecnico (Milan). From 1986 he worked at Pierrel (Milan) on heterocyclic NSAIDs; at Marion Merrell Dow, on semisynthetic modification of natural antibacterials (Gerenzano), and on neuroprotective agents (Strasbourg); at Selectide (Tucson, USA) on combinatorial libraries of natural product-like structures; at SmithKlineBeecham (Rennes) as Lab Head of Chemistry, working in oncology and osteoporosis; and at GlaxoWellcome (Verona) as Director of Lead Discovery, leading the optimization of antibacterial and CNS agents. In 2000 he was a co-founder and CSO of NADAG (Munich), working on disease-modifying agents to cure AD.
In 2003 he became Associate Professor at the University of Milan, where he teaches basic and advanced courses. His medicinal chemistry interests are in oncology (pro-apoptotics, natural product derivatives, immuno-oncology) and in neurodegeneration (disease-modifyers against AD, PD and ALS). He authored more than 120 papers, 15 patents and 4 books.

Dr Luca Muzio, San Raffaele Scientific Institute, Italy

Dr Luca Muzio, San Raffaele Scientific Institute, Italy
Luca Muzio received his degree in Biology in Genoa. He is a senior scientist at the Institute of Experimental Neurology (INSpe) of San Raffaele Scientific Institute, Italy. He is a trained biologist that completed his PhD in 2005, working in the field of developmental biology. It is in that context that he investigated transcription factors and molecular mechanisms involved in cortical development. In 2006, he joined the INSpe and he has made research contributions in the field of neuroimmunology. He carried out different types of experiments and researches on animal models of multiple sclerosis (MS). More recently, he started to investigate neurodegeneration in Amyotrophic Lateral Sclerosis (ALS). He did researches focused on microglia activation in ALS models and recently he started to investigate the retromer molecular pathway. Starting from 2015, he teaches at the University Vita Salute of Milan.

Dr Justin Ichida, University of Southern California, USA

Dr Justin Ichida, University of Southern California, USA
Justin K Ichida is an Associate Professor of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC. Prior to joining USC, Dr Ichida earned his PhD at Harvard Medical School studying the origins of life with Jack Szostak and did postdoctoral work on cellular reprogramming with Kevin Eggan at Harvard University.
Dr Ichida conducts research on the etiology, pathogenesis, genetics, and treatment of neurodegenerative diseases, with a focus on amyotrophic lateral sclerosis (ALS) and frontotemporal dementia. His work has garnered many awards, including a Pathway to Independence Award from the National Institutes of Health, the New York Stem Cell Foundation Innovator Award, the Richard N. Merkin Scholar Award, and the Donald and Delia Baxter Foundation Faculty Scholar Award. In December 2017, Ichida received the Champion for a Cure Award from the ALS Association, the highest honor the ALS Association bestows on scientists for distinguished intellectual achievements.
Since starting at USC in 2013, Dr Ichida has secured more than $15 million in external funding for research on ALS, frontotemporal dementia, Alzheimer’s disease, and other disorders of the nervous system. Ichida has published 68 scientific papers in the scientific literature and has co-founded a Los Angeles-based biotech company to translate findings from his lab to the clinic.
| 16:00 - 17:00 |
Early career 'table' discussions

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, Canada

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, CanadaPeter St George-Hyslop FRS is a medical scientist, neurologist and molecular geneticist who is distinguished for his research into neurodegenerative disorders, including Alzheimer’s disease (AD). In particular, he discovered several genes that when mutated lead to early onset hereditary AD, accelerating our understanding the disease and the development of potential treatments. His discovery that defective genes encoding presenilins are a cause of familial AD led to presenilins becoming a new target for treatments. He went on to show that mutated presenilins contribute to the generation of the amyloid beta protein — deposition of which is the earliest sign of AD in those carrying such genes. His work on several other neurodegeneration-related genes and proteins (including SORLA, TREM2, FUS and ANXA11) has led to an understanding of the role of vesicular transport, inflammation and perturbed RNA granule biology. Peter has led an AD research programme as Professor of Experimental Neuroscience at the University of Cambridge since 2007. He was awarded the Howard Hughes Medical Institute International Scholar Award in both 1997 and 2002, and has received several other notable awards. 
Dr Justin Ichida, University of Southern California, USA

Dr Justin Ichida, University of Southern California, USAJustin K Ichida is an Associate Professor of Stem Cell Biology and Regenerative Medicine at the Keck School of Medicine of USC. Prior to joining USC, Dr Ichida earned his PhD at Harvard Medical School studying the origins of life with Jack Szostak and did postdoctoral work on cellular reprogramming with Kevin Eggan at Harvard University. Dr Ichida conducts research on the etiology, pathogenesis, genetics, and treatment of neurodegenerative diseases, with a focus on amyotrophic lateral sclerosis (ALS) and frontotemporal dementia. His work has garnered many awards, including a Pathway to Independence Award from the National Institutes of Health, the New York Stem Cell Foundation Innovator Award, the Richard N. Merkin Scholar Award, and the Donald and Delia Baxter Foundation Faculty Scholar Award. In December 2017, Ichida received the Champion for a Cure Award from the ALS Association, the highest honor the ALS Association bestows on scientists for distinguished intellectual achievements. Since starting at USC in 2013, Dr Ichida has secured more than $15 million in external funding for research on ALS, frontotemporal dementia, Alzheimer’s disease, and other disorders of the nervous system. Ichida has published 68 scientific papers in the scientific literature and has co-founded a Los Angeles-based biotech company to translate findings from his lab to the clinic. 
Professor Pierfausto Seneci, University of Milan, Italy

Professor Pierfausto Seneci, University of Milan, ItalyPierfausto Seneci received his degree in Chemistry in Pavia, followed by a postdoc at Politecnico (Milan). From 1986 he worked at Pierrel (Milan) on heterocyclic NSAIDs; at Marion Merrell Dow, on semisynthetic modification of natural antibacterials (Gerenzano), and on neuroprotective agents (Strasbourg); at Selectide (Tucson, USA) on combinatorial libraries of natural product-like structures; at SmithKlineBeecham (Rennes) as Lab Head of Chemistry, working in oncology and osteoporosis; and at GlaxoWellcome (Verona) as Director of Lead Discovery, leading the optimization of antibacterial and CNS agents. In 2000 he was a co-founder and CSO of NADAG (Munich), working on disease-modifying agents to cure AD. In 2003 he became Associate Professor at the University of Milan, where he teaches basic and advanced courses. His medicinal chemistry interests are in oncology (pro-apoptotics, natural product derivatives, immuno-oncology) and in neurodegeneration (disease-modifyers against AD, PD and ALS). He authored more than 120 papers, 15 patents and 4 books. 
Dr Luca Muzio, San Raffaele Scientific Institute, Italy

Dr Luca Muzio, San Raffaele Scientific Institute, ItalyLuca Muzio received his degree in Biology in Genoa. He is a senior scientist at the Institute of Experimental Neurology (INSpe) of San Raffaele Scientific Institute, Italy. He is a trained biologist that completed his PhD in 2005, working in the field of developmental biology. It is in that context that he investigated transcription factors and molecular mechanisms involved in cortical development. In 2006, he joined the INSpe and he has made research contributions in the field of neuroimmunology. He carried out different types of experiments and researches on animal models of multiple sclerosis (MS). More recently, he started to investigate neurodegeneration in Amyotrophic Lateral Sclerosis (ALS). He did researches focused on microglia activation in ALS models and recently he started to investigate the retromer molecular pathway. Starting from 2015, he teaches at the University Vita Salute of Milan. 
Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The Netherlands

Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The NetherlandsHenne Holstege is an Associate Professor at the Amsterdam University Medical Center. After she majored in biochemistry at the University of Leiden she did her PhD at the Netherlands Cancer Institute. During this time Dr Holstege was intrigued by the extraordinary case of a Dutch woman who died at age 115 without any symptoms of cognitive decline because this woman proved that cognitive decline is not inevitable. Holstege set up the 100-plus Study, a cohort study of cognitively healthy centenarians to identify protective genetic and biomolecular factors that associate with the escape of cognitive decline. She analyses the data from the centenarians in context of the genetics and biomolecular factors of (early onset) Alzheimer’s Disease; both extremes on the same cognitive spectrum. Therefore, her lab is involved in large international collaborative joint analysis of sequencing data thousands of Alzheimer Disease cases and cognitively healthy controls the collected by European ADES and American ADSP consortia. Holstege and collaborators are currently identifying novel genes associated with the increased or decreased risk of AD. Here, she applies specific focus on the identification of rare pathogenic variants in the SORL1 gene, which next to APOE-e4 allele, is the most common and strongest risk factor of AD. One of her major goals is, therefore, is to implement adequate clinical counselling strategies of SORL1 variant to the carriers and their family members. For this reason, a part of her lab is embedded in the clinic, and involved in counseling genetically predisposed Alzheimer Disease patients. For her work, Holstege was awarded the Alzheimer Research Prize by the Hans und Ilse Breuer Foundation in 2020. For more information see: www.holstegelab.eu. |
|---|
