Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Understanding the endosomal network in neurodegeneration
Scientific discussion meeting organised by Professor Peter Cullen, Professor Peter St George-Hyslop FRS, Professor Scott Small and Dr Henne Holstege.
Abnormalities in the endosomal network are a signature feature of Alzheimer's disease, Parkinson's disease and numerous other neurological disorders. In bringing together world leading researchers from a range of disciplines, this meeting sought to discuss the latest advances in this rapidly moving field and foster collaborative efforts to enhance the rate of discovery in this medically important research field.
The schedule of talks and speaker biographies are available below. Speaker abstracts are also available below.
Attending this event
This meeting has taken place.
Enquiries: contact the Scientific Programmes team.
Click watch on YouTube to view the full video playlist.
Organisers
Schedule
Chair

Professor Bart De Strooper, UK Dementia Research Institute, University College London, VIB and KU Leuven Belgium

Professor Bart De Strooper, UK Dementia Research Institute, University College London, VIB and KU Leuven Belgium
Professor Bart De Strooper is the founding director of the UK Dementia Research Institute (UK DRI). He is a researcher in Alzheimer's disease, and supervises laboratories based in the UK DRI at the Francis Crick Institute in London and in the VIB laboratory at the KU Leuven in Belgium. Bart De Strooper’s research is focused on translating genetic findings into mechanisms of neurodegenerative diseases and drug targets. He is best known for his work on the presenilins and gamma-secretase, and more recently for his work on the cellular theory of Alzheimer’s Disease. He was elected to the Academy of Medical Sciences Fellowship in 2020, and has received several awards including the Potamkin prize, the Metlife Foundation Award for Medical Research, Alois Alzheimer’s prize, the highly prestigious Brain Prize 2018 and Commander in the Order of Leopold I.;

Dr Kirsty McMillan, University of Bristol, UK

Dr Kirsty McMillan, University of Bristol, UK
Throughout her career Kirsty has developed a wide breadth of knowledge across biochemistry, neuroscience, and pharmacology to understand the molecular mechanisms driving neurodegeneration. Kirsty was awarded her BBSRC Industrial Collaborative PhD from the University of Bristol in Professor Maeve Caldwell’s lab in 2014. Her research investigated the role of microRNAs on the regulation of alpha synuclein expression. Since then, Kirsty has worked in the lab of Professor Peter Cullen at the University of Bristol, where she is currently a Research Fellow. Her research has focused on understanding the role of the endosomal system in neuronal and glial function, and in neurodegenerative disease.
| 09:00 - 09:05 | Welcome |
|---|---|
| 09:05 - 09:25 |
Genetic risk, consequences, and rescue of rab5-endosome dysfunction in Alzheimer’s Disease
Preceding any other neuropathology in Alzheimer’s Disease (AD) brain, neuronal early endosomes (EE) enlarge more than two-fold in response to abnormal activation of Rab 5 GTPase and upregulated transcription of Rab5 effectors. This Rab5 'phenotype' is selective for AD, both late onset and familial early onset subtypes linked to APP, including Down syndrome (DS). The EE phenotype on primary DS fibroblasts and AD/DS mouse models depends on elevated levels of APP-βCTF and not Aβ. APP-βCTF recruits the adaptor protein APPL1 to endosomes where it stabilises the activated state of rab5, thus linking βCTF directly to AD-related rab5 hyper-activation. APPL1 KD abrogates these events in neurons of DS-model mice, while its over-expression in wt mice enlarges Rab5-endosomes, as expected. Notably, gene polymorphisms conferring increased AD risk, including APOE4, SORL1, RIN3 etc. also hyper-activate Rab5 and enlarge EE, in some cases independently of APP-βCTF. Extent of endosome swelling correlates with their slower rates and stalling during axonal/dendritic transport to the nucleus, including endosomes carrying NGF responsible for cholinergic neuron survival. Basal forebrain cholinergic neuron (BFCN) degeneration in APP-based AD models is reversed by lowering APP-βCTF or rab5 over-activation. Reproducing neuronal rab5 activation in mice phenocopies pathological consequences seen in DS model mice: EE enlargement and impaired axonal transport, tau hyperphosphorylation, LTP deficits, dendritic spine atrophy, BFCN neurodegeneration, and cognitive deficit. Neflamapimod (NFMD), a p38alpha kinase inhibitor that blocks rab5 hyper-activation at sub-micromolar concentrations, reverses the foregoing phenotype in DS model mice. A phase 2 clinical trial of NFMD in Lewy Body Dementia, NFMD improved cognitive and motor impairments attributable to prominent BFCN deficits in LBD. Support: NIA. 
Professor Ralph A Nixon, New York University Langone Medical Centre, USA

Professor Ralph A Nixon, New York University Langone Medical Centre, USADr. Nixon received his PhD from Harvard University, MD from University of Vermont, and training in medicine and psychiatry at Massachusetts General Hospital. He is a Fellow of the American College of Neuropsychopharmacology. Dr. Nixon’s pioneering research first established the importance of proteases and defective proteolytic systems in the pathogenesis of Alzheimer’s disease and has identified new therapeutic approaches for the disease. Dr. Nixon has over 300 scientific papers (H-index, 114) and eight issued patents. He served as chair of the Neuroscience, Behavior and Sociology of Aging Review Committee at NIH, Chair of the Medical and Scientific Advisory Council of the Alzheimer’s Association and member of its Board of Directors, and currently serves on the Governor’s Commission on Alzheimer’s Disease for New York State. Dr. Nixon’s awards include the MERIT, Leadership and Excellence in Alzheimer Research(LEAD), and Academic Career Leadership Awards from NIH and the Zenith, Temple Discovery, and Khachaturian Awards from the Alzheimer’s Association. |
| 09:25 - 09:35 | Discussion |
| 09:35 - 09:55 |
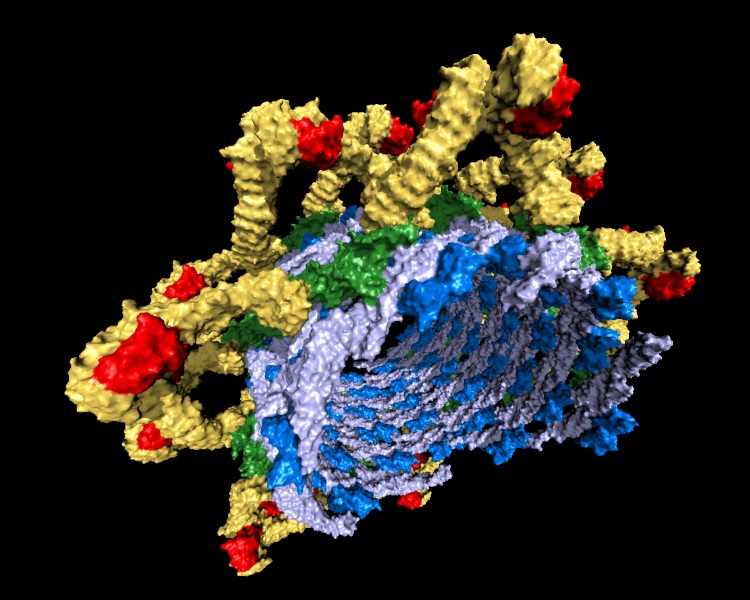
Towards a thorough molecular understanding of endosomal cargo sorting in health and disease
Professor Cullen's laboratory has sought to define the molecular machinery that serve to orchestrate the sorting of receptors, channels, transporters, polarity and adhesion molecules, and their associated proteins and lipids (collectively termed ‘cargoes’), through the endosomal network. Using structural and biochemical approaches coupled with in cellulo and in vivo analysis they have identified several evolutionary conserved multiprotein assemblies that conduct cargo sorting through the network, including human SNX3-Retromer and SNX27-Retromer complexes. This has provided new insight into cellular processes including nutrient sensing and signalling, cell adhesion and migration, and structural and functional synaptic plasticity, and has, in turn, begun to reveal how deregulation of endosomal sorting is associated with human disease. A current major focus is to apply an array of organelle-restricted proteomic approaches to unbiasedly quantify the global effect of retromer perturbation on the function of neurons and supporting cells within the context of brain development and age-related neurodegenerative disease. Read the preprint report. 
Professor Peter Cullen, University of Bristol, UK

Professor Peter Cullen, University of Bristol, UKBiography not available |
| 09:55 - 10:05 | Discussion |
| 10:05 - 10:25 |
Integrative biology and neurodegenerative diseases: the case of SORL1-retromer and Alzheimer’s disease
The complexity, inaccessibility to experimentation of the human brain, lack of good animal models, and phenotypic heterogeneity and age dependence of most neurodegenerative diseases make finding causal pathways very difficult. Professor Petsko presents specific criteria to establish causality and validate a target and therapeutic approach. Given the complexity of the problem, such criteria should reflect an integrative biology approach: combining information and experiments from human genetics (are there causal mutations in the pathway?), molecular biology (are key molecules in the pathway dysregulated in the disease?), cellular biology (when disrupted, does the pathway cause the disease’s cardinal cellular pathologies, and can they be mediated by renormalising the pathway?), and anatomical biology (when disrupted, does the pathway cause the disease’s cardinal anatomical pathology?). Professor Petsko applies these criteria, Koch’s Postulates for Neurodegenerative Diseases if you will, to the endosomal trafficking pathway regulated by the retromer multi-protein assembly. In conjunction with the retromer cargo receptor SORLA (product of the SORL1 gene), this pathway satisfies the integrative biology criteria: (1) rare alleles of SORL1 are causal for familial AD that phenocopies the common form; (2) retromer is deficient in the brains of both familial and sporadic AD patients; (3) disruption of SORL1-retromer dependent trafficking recapitulates the cardinal cellular pathologies of the disease in both patient-derived neurons and animals, and increasing retromer function rescues them; and (4) disruption of SORL1-retromer trafficking in animals causes synaptic dysfunction leading to neurodegeneration in the trans-entorhinal cortex, where AD pathology usually begins in the human disease. Professor Petsko therefore proposes the SORL1-retromer trafficking pathway as causal in many, if not most, cases of Alzheimer’s disease. Targeting this pathway may be of considerable therapeutic benefit. 
Professor Gregory Petsko, Ann Romney Center for Neurologic Diseases,Harvard Medical School and Brigham & Women’s Hospital, USA

Professor Gregory Petsko, Ann Romney Center for Neurologic Diseases,Harvard Medical School and Brigham & Women’s Hospital, USAGregory A Petsko is Professor of Neurology in the Ann Romney Center for Neurologic Diseases at Harvard Medical School and Brigham & Women’s Hospital in Boston, and Adjunct Professor of Biomedical Engineering at Cornell University. He has been elected to the National Academy of Sciences, the National Academy of Medicine, the American Academy of Arts and Sciences, and the American Philosophical Society. He is a past president of the American Society for Biochemistry and Molecular Biology and of the International Union of Biochemistry and Molecular Biology. He has founded several publicly traded and private companies and serves on the advisory boards of MeiraGTx, Retromer Therapeutics, Amicus Therapeutics, Proclara Biosciences, and Annovis Bio. His work aims to develop treatments for neurodegenerative diseases, including ALS, Alzheimer’s, and Parkinson’s. His public lectures on brain health have attracted a wide audience (one of his TED talks has been viewed over a million times). He has also written a widely-read column on science and society, the first ten years of which are available in book form. He admits, however, that the columns guest-written by his two dogs, Mink and Clifford, are more popular than those he writes himself. |
| 10:25 - 10:35 | Discussion |
| 10:35 - 11:00 | Coffee |
| 11:00 - 11:10 |
Selected presentation
Endolysosomal dysfunction as a converging mechanism in FTLD spectrum disorders Christy Hung and Rickie Patani The Francis Crick Institute, UK Amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD) were traditionally considered as two distinct neurodegenerative diseases which affect motor neurons and frontotemporal lobes, respectively. However, accumulating evidence suggests some convergence in molecular and genetic pathology, which may argue against their taxonomy as completely distinct entities. The valosin-containing protein (VCP/p97) gene is highly relevant, being associated with both FTD and ALS. Yet, the overlapping pathogenic pathways shared by both forms of the disease have remained unclear. This question is important because it provides clues to the most critical steps for therapeutic targeting. To address this, human induced pluripotent stem cells (iPSCs) carrying VCP mutations, which are causal for familial ALS and FTD, are directly differentiated into highly enriched and functionally validated cortical neurons and spinal cord motor neurons. Mutations in VCP lead to abnormal accumulation of enlarged endosomes, major defects in lysosomal function and defective axonal lysosome transport in both cortical and motor neurons. Taken together, these results suggest that the dysfunction of the endolysosomal-autophagic system represents a convergent mechanism shared by ALS and FTD. |
| 11:10 - 11:15 | Discussion |
| 11:15 - 11:25 |
Selected presentation
Electron cryo-tomography of human iPSC-derived neurons to study structural changes in Alzheimer’s disease Bronwen Foster1,2, Michael Grange1, Selina Wray2 and Charles Arber2
1Rosalind Franklin Institute, UK The endosomal lysosomal network (ELN) is disrupted in a variety of neurodegenerative diseases. In Alzheimer’s disease (AD), structural changes in the ELN have been described as the earliest documented AD-specific changes in mouse models and human neurons, specifically increased fusion and enlargement of Rab5 endosomes. Amyloid precursor protein (APP) processing occurs in endosomes, and APP-β C-terminal fragments directly over-activate Rab5, causing increased endocytosis and defects in endosome-mediated trafficking and signalling. This directly links aberrant APP processing and dysfunction of the ELN. Structural insight into these subcellular changes is required to appreciate the early molecular changes governing the AD mechanism. Electron cryo-tomography (cryo-ET) is an in-situ technique enabling visualisation of intracellular structures in their native context of the cell. This technique is being used to investigate cortical neurons derived from induced pluripotent stem cells (iPSC) harbouring mutations in APP and PSEN1 which are causative of familial AD. iPSC-derived cortical neurons can be grown on electron microscopy grids, allowing specific structures to be targeted using multi-modal approaches. AD-specific ELN defects visualised in situ in a variety of AD patient-derived iPSC lines will provide insight into the earliest fundamental molecular changes in the AD mechanism. |
| 11:25 - 11:30 | Discussion |
| 11:30 - 11:50 |
The trans-entorhinal cortex differential relies on a distinct retromer core dedicated to endosomal recycling
Anatomical studies have pinpointed the trans-entorhinal cortex (TEC) as one of the subregions within the brain most vulnerable to Alzheimer’s disease (AD). Interestingly, endosomal trafficking defects have now become a well-accepted feature of AD, based on a growing body of evidence from genetic, molecular, and biology studies. However, whether and how endosomal trafficking is linked to anatomical vulnerability still remains unclear. Here, in addressing these questions, the group began by showing that neurons are enriched with a functional distinct retromer core organized around VPS26b, differentially dedicated to endosomal recycling. Using fMRI imaging, and in contrast to its paralog VPS26a, the group further demonstrated that depleting VPS26b in mice caused a specific and age-dependent dysfunction in the TEC region, a finding further validated by electrophysiology, immunocytochemistry, and behaviour. Surprisingly, repletion of VPS26b, both in vitro and in vivo, rescued the phenotypes seen upon VPS26b deficiency, further supporting the relevance of VPS26b for the proper functioning of the TEC region. Additionally, when the group turned to humans, VPS26b was found highly enriched in the TEC region of healthy control individuals, and reduced – together with retromer-related receptor SORL1 – in patients with AD. Finally, by regulating glutamate receptor and SORL1 recycling and its levels, VPS26b was shown to mediate regionally-selective synaptic dysfunction, as well as AD-associated amyloid-precursor protein misprocessing and tau secretion. Together with the trans-entorhinal’s unique network properties, hypothesized to impose a heavy demand on endosomal recycling, our results contribute to the overall hypothesis explaining AD’s regional vulnerability. 
Dr Sabrina Simoes, Columbia University, USA

Dr Sabrina Simoes, Columbia University, USADr Simoes is a cellular neurobiologist who has spent her career studying endosomal trafficking in normal and pathological conditions. Research in her lab focus on understanding the mechanisms underlying the pathogenesis of Alzheimer’s disease (AD), with special emphasis on endo-lysosomal dysfunction. Dr Simoes received her PhD in cell biology from the Institute Curie and University Paris Descartes, France. During her training in Dr Raposo’s lab – a world leader in the exosome/endosome field – she developed a strong interest in intracellular trafficking. Her early studies focused on how endosomal machineries are explored by Prions for their sorting into exosomes and concomitant spread, as well as for endosome maturation. In 2011, she joined Dr Small’s laboratory at Columbia University, where she continued to pursue her studies on endosomal trafficking in the context of neurodegeneration. In 2019 she was promoted to Assistant Professor in the Department of Neurology and the Taub Institute. She is currently Principal Investigator on several NIH and private funded studies aimed at developing new biomarkers for AD and other neurodegenerative disorders, focus on endosomal dysfunction. Lastly, she leads the biofluid component of the Biomarker Core at Columbia's ADRC. |
| 11:50 - 12:00 | Discussion |
| 12:00 - 12:20 |
The neuronal retromer regulates the endosomal network and modulates both neuronal and microglial phenotypes of Alzheimer's Disease
Disruption of retromer-dependent endosomal trafficking is considered pathogenic in late-onset Alzheimer's disease (AD). Here, to investigate this disruption in the intact brain, Dr Qureshi turns to a genetic mouse model where the retromer core protein VPS35 is depleted in hippocampal neurons, and then he repletes VPS35 using an optimised viral vector protocol. The VPS35 depletion-repletion studies strengthen the causal link between the neuronal retromer and AD-associated neuronal phenotypes, including the acceleration of amyloid precursor protein cleavage and the loss of synaptic glutamate receptors. Moreover, the studies show that the neuronal retromer can regulate a distinct, dystrophic, microglia morphology, phenotypic of hippocampal microglia in AD. Finally, the neuronal and, in part, the microglia responses to VPS35 depletion were found to occur independent of tau. Showing that the neuronal retromer can regulate AD-associated pathologies in two of AD's principal cell types strengthens the link, and clarifies the mechanism, between endosomal trafficking and late-onset sporadic AD. 
Dr Yasir H Qureshi, Columbia University, USA

Dr Yasir H Qureshi, Columbia University, USADr Qureshi is a neuroscientist trained at Columbia University, New York. His research focuses on the molecular pathways and genetic variations that contribute to Alzheimer’s disease’s pathology. He is investigating novel pathological pathways to identify potential therapeutic targets, and exploit them using drug and genetic interventions to achieve clinical remission of AD. Dr Qureshi is using mouse models of endosomal/retromer dysfunction and AAV viral vectors as biological and therapeutic tools for altering levels of different retromer complex proteins in the brain in an attempt to improve trafficking through the endosomal system. He is further exploring the role of retromer in physiological/pathological processing of proteins and its downstream effects on Alzheimer disease progression, hippocampal plasticity and memory formation. In a recent report he has demonstrated that neuronal-specific endosomal deficits can result in misprocessing of amyloid precursor protein and degradation of glutamate receptors in neurons; in addition to this the endosomal dysfunction in neurons leads to astrocytic activation and an AD-like dystrophic morphology of hippocampal microglia. Dr Qureshi is developing gene therapy programs around different components of the endosomal trafficking machinery and working closely on this with a new biotechnology company, Retromer Therapeutics. |
| 12:20 - 12:30 | Discussion |
Chair
Professor Scott Small, Columbia University, USA
Professor Scott Small, Columbia University, USA
Scott A. Small MD is the Director of the Alzheimer’s Disease Research Center at Columbia University, where he also directs the Psychosis Research Program.
Dr. Small focuses on disorders that affect the hippocampus, a brain structure targeted by Alzheimer’s disease, schizophrenia, and the normal wear & tear of the aging process. The hippocampus is a circuit comprised of a handful of microscopic regions. The overarching hypothesis motivating Dr. Small’s lab is that if hippocampal regions most vulnerable to a disorder can be pinpointed, this anatomical information can guide a search for the disorder’s root cause.
Accordingly, Dr. Small’s ‘anatomical biology’ lab has pioneered the development of MRI tools best suited to isolate vulnerable hippocampal regions. His lab has then used this information to identify mechanisms that are now thought to underlie Alzheimer’s disease, schizophrenia, and ‘cognitive aging’. Most recently, his lab has begun developing interventions for each condition. To date, the lab has completed two clinical trials for cognitive aging and one for schizophrenia, and the lab’s Alzheimer’s disease findings was the cornerstone around which a new biotechnology company, Retromer Therapeutics. was formed.
| 13:30 - 13:50 |
Functions of the neuronal endolysosomal system in tauopathy initiation and progression
Tauopathies, including Alzheimer’s disease and frontotemporal dementia, share the feature of apparent spatial spreading through neural networks, between diseased and healthy neurons. In this presentation, Professor Livesey will discuss the contribution of the endolysosome system to inter-neuronal transfer of pathogenic forms of microtubule-associated tau protein. Endolysosome dysfunction is emerging as an important pathogenic process in tauopathies, influencing both disease initiation and progression through the CNS. Autosomal dominant mutations in PSEN1 and APP causal for Alzheimer’s disease compromise human neuronal endolysosome function and autophagy. This results in extracellular release of cleaved forms of tau protein that contain the aggregation-prone microtubule-binding region (MTBR), which are efficiently taken up by neurons via LRP1-mediated endocytosis, which Professor Livesey proposes contributes to disease propagation. Whole genome CRISPR knockout screens in human neurons were used to identify the genes and pathways required for uptake of extracellular tau. In addition to identifying surface receptors for tau and routes for tau’s receptor-mediated endocytosis, the group found that the large multifunctional protein LRRK2 is a key regulator of neuronal tau endocytosis. Given LRRK2’s role in Parkinson’s disease pathogenesis, Professor Livesey will discuss the possible similarities in disease mechanisms involving the endolysosome system between tauopathies and other neurodegenerative diseases. 
Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UK

Professor Rick Livesey, UCL/Great Ormond Street Institute of Child Health, UKRick Livesey is Professor of Stem Cell Biology at the UCL/Great Ormond Street Institute of Child Health. He is also head of the Genetic and Neurodevelopmental Disorders Research Unit at Biogen, and scientific founder of two biotech spinouts based in Cambridge, Talisman Therapeutics and Gen2 Neuroscience. Prior to joining UCL in 2018, he was a Senior Group Leader at the Wellcome Trust/Cancer Research UK Gurdon Institute at the University of Cambridge. His research focuses on the cell and molecular biology of neurodegenerative disease, with particular interest in genetic diseases of the cerebral cortex in children and adults and the development of novel therapeutics for those conditions.
|
|---|---|
| 13:50 - 14:00 | Discussion |
| 14:00 - 14:20 |
Cell-type specific actions of the SORL1-retromer axis in human neural cells
Dysfunction in the endo-lysosomal network (ELN) is an early driver of Alzheimer’s disease pathogenesis and therapeutics targeting this pathway could be novel and effective. However, understanding how the ELN functions in the diverse cell types of the brain and how ELN genes that confer increased AD risk modulate these functions are necessary. The group uses human induced pluripotent stem cell-derived neurons and glia to elucidate the role of the sorting receptor SORL1, an established AD risk gene, in ELN function. SORL1 is an adaptor that interacts with the multi-protein sorting assembly, retromer, to traffic cellular cargo. The most characterized cargo sorted by SORL1-retromer is the amyloid precursor protein APP. The data indicates that in neurons, loss of SORL1 function converges on the early endosome, leading to endosome enlargement and mislocalization of several important neuronal cargo, including neurotrophin receptors and subunits of post-synaptic complexes. These 'traffic jams' have an impact on localization of synaptic machinery and neuronal function. In microglia, they demonstrate that loss of SORL1 impacts the lysosome, inducing lysosomal enlargement, impairing lysosomal enzymes and degradation of phagocytosed substrates. Finally, they show that enhancement of retromer function via a small molecules can rescue ELN dysfunction in neurons, however the degree of phenotypic rescue depends on whether there is a functional copy of SORL1 in the cell. Using a disease-relevant preclinical model, our work illuminates how the SORL1-retromer pathway can be therapeutically harnessed. 
Dr Jessica Young, University of Washington, USA

Dr Jessica Young, University of Washington, USAJessica Young received her PhD in Molecular and Cell Biology in 2009 from the University of Washington in the laboratory of Dr Albert La Spada where she studied the role of autophagy in neurodegenerative disease. She pursued postdoctoral training with Dr Lawrence SB Goldstein at the University of California, San Diego where she focused on developing human induced pluripotent stem cell (hiPSC) models of Alzheimer’s disease. She is currently an Assistant Professor in the Department of Laboratory Medicine and Pathology at the University of Washington where, since 2016, her laboratory is working to understand the role of AD risk genes in neuronal endo-lysosomal dysfunction using patient derived and gene-edited hiPSCs. The Young lab is dedicated to building accurate in vitro models of neurodegenerative disease and understanding cell biological mechanisms the lead to disease pathogenesis. Current funded projects in the lab include 1) understanding the role of SORL1 in endo-lysosomal trafficking in hiPSC-derived neurons, microglia, and brain organoids and 2) elucidating epigenetic mechanisms that regulate neuronal metabolism and ageing. Dr Young’s research is funded by the BrightFocus Foundation and the NIH (NIA). |
| 14:20 - 14:30 | Discussion |
| 14:30 - 14:40 |
Selected presentation
TMCC2, an apoE and APP-interacting endolysosomal protein, associates with Alzheimer’s disease pathology in the human brain. Paul CR Hopkins, Claire Troakes, Andrew King and Guy Tear Transmembrane and Coiled-Coil 2 (TMCC2) is an ER and endolysosome-associated protein that forms complexes with both apolipoprotein E (apoE) and the amyloid protein precursor (APP), two proteins central to the aetiology of Alzheimer’s disease (AD). Mutation of Drosophila TMCC2 (Dementin) can cause neurodegeneration with features of AD, ie accumulation of fragments of the APP-Like protein, synaptogenic defects, mis-localisation of cytoskeletal proteins and early death.
Here the investigators report the first investigation of TMCC2 in AD cases associated with apoE, mutations in APP Val717, and Down syndrome. TMCC2 and APP immunoreactivities are closely associated in neurons of both control and late onset AD cases. In all AD cases TMCC2 immunoreactivity was associated with dense core plaques and adjacent dystrophic neurites, but not with amyloid surrounding the core, nor with diffuse amyloid plaques or neurofibrillary tangles. In Down syndrome neuritic plaques, TMCC2 immunoreactivity additionally co-localized with amyloid having a spicular or threadlike pattern not seen in the non-Down syndrome cases examined. Western blot revealed that TMCC2 exists as at least three protein isoforms, the relative abundance of which varied between the temporal gyrus and cerebellum, and was influenced by APOE genotype and/or dementia status. |
| 14:40 - 14:45 | Discussion |
| 14:45 - 14:55 |
Selected presentation
Mutations in two Parkinsonism-linked endocytic genes SYNJ1 and DNAJC6 have synergistic effects on dopaminergic axonal pathology Xin Yi Ng1, Yumei Wu2*, Youneng Lin1*, Sidra Mohamed Yaqoob1*, Lois E Greene3, Pietro De Camilli2 and Mian Cao1,4 1Programme in Neuroscience and Behavioural Disorders, Duke-NUS Medical School, Singapore *These authors contributed equally Parkinson’s disease (PD) is a neurodegenerative disorder characterised by defective dopaminergic (DAergic) input to the striatum. Mutations in two genes encoding synaptically-enriched clathrin-uncoating factors, synaptojanin 1 (SJ1) and auxilin, have been implicated in atypical Parkinsonism. SJ1 knock-in (SJ1-KIRQ) mice carrying a disease-linked mutation display neurological manifestations reminiscent of Parkinsonism. Here Dr Cao’s group reports that auxilin knockout (Aux-KO) mice display dystrophic changes of a subset of nigrostriatal DAergic terminals similar to those of SJ1-KIRQ mice. Furthermore, Aux-KO/SJ1-KIRQ double mutant mice have shorter lifespan and more severe synaptic defects than single mutant mice. These include increase in dystrophic striatal nerve terminals positive for DAergic markers and for the PD risk protein SV2C, as well as adaptive changes in striatal interneurons. The synergistic effect of the two mutations demonstrates a special lability of DAergic neurons to defects in clathrin uncoating, with implications for PD pathogenesis in at least some forms of this condition. |
| 14:55 - 15:00 | Discussion |
| 15:00 - 15:20 |
Dimerisation of the Alzheimer’s disease pathogenic receptor SORLA regulates its association with retromer
SORL1, the gene encoding the large multi-domained SORLA protein, has emerged as only the fourth gene that when mutated can by itself cause Alzheimer’s disease (AD), and as a gene reliably linked to both the early- and late-onset forms of the disease. SORLA is known to interact with the endosomal trafficking regulatory complex called retromer in regulating the recycling of endosomal cargo, including the amyloid precursor protein (APP) and the glutamate receptor GluA1. Nevertheless, SORLA’s precise structural-functional relationship in endosomal recycling tubules remains unknown. Here Dr Andersen addresses these outstanding questions by relying on crystallographic and artificial-intelligence evidence to generate a structural model for how SORLA folds and fits into retromer-positive endosomal tubules, where it is found to dimerise via both SORLA’s fibronectin-type-III (3Fn)- and VPS10p-domains. Moreover, he identifies a SORLA fragment comprising the 3Fn-, transmembrane, and cytoplasmic domains that has the capacity to form a dimer, and to enhance retromer-dependent recycling of APP by decreasing its amyloidogenic processing. Collectively, these observations generate a model for how SORLA dimer (and possibly polymer) formation can function in stabilising and enhancing retromer function at endosome tubules. These findings can inform investigation of the many AD-associated SORL1 variants for evidence of pathogenicity and can guide towards discovery of novel drugs for the disease. 
Dr Olav Andersen, Aarhus University, Denmark

Dr Olav Andersen, Aarhus University, DenmarkOlav Andersen graduated from Aarhus University in 2001, followed by 6 years as postdoctoral researcher at the Max-Delbrück-Center for molecular medicine in Berlin, before he returned to Aarhus University to become associate professor and establishing his research group focusing on SORL1 and Alzheimer’s disease. |
| 15:20 - 15:30 | Discussion |
| 15:30 - 16:00 | Tea |
| 16:00 - 16:20 |
Loss of NPC1 in myeloid cells drives astrogliosis and neuronal pathology
Microglial activation is a neuropathological hallmark of the lysosomal storage disease Niemann-Pick type C (NPC). Whole-body knockout of NPC1 results in enhanced phagocytic uptake and impaired myelin turnover in microglia that precede neuronal death. Npc1-deficient microglia are characterized by accumulation of multivesicular bodies and impaired intracellular trafficking of lipids to lysosomes while lysosomal degradation remains preserved. To study a cell-autonomous function of NPC1 in microglia, the group generated a conditional knock-out of NPC1 in myeloid cells by crossing Npc1flox/flox mice with Cx3cr1+/Cre mice and characterized microglial, astrocytic and neuronal phenotypes by PET imaging, immunohistochemistry and mass spectrometry at different pathological stages (8 weeks, 7 months and 12 months). Microglial activation was the first pathological alteration detected in the brain upon loss of NPC1 in myeloid cells (8 weeks of age), accompanied by disease-associated microglial signatures. Starting from an age of 7 months, microgliosis was followed by astrogliosis that were detected by TSPO-PET and Deprenyl-D2-PET imaging, respectively. Furthermore, the loss of microglial NPC1 triggered neuronal injuries (axonal spheroids) as well as motor defects (rotarod) at the age of 7 months.This work reveals that a specific loss of NPC1 in myeloid cells is sufficient to trigger pathology in other brain cells, suggesting that a pathological cascade initiated by microglial dysfunction may propagate to astrocytes and neurons. 
Dr Sabina Tahirovic, Deutsches Zentrum für Neurodegenerative Erkrankungen e. V. (DZNE), Germany

Dr Sabina Tahirovic, Deutsches Zentrum für Neurodegenerative Erkrankungen e. V. (DZNE), GermanySabina Tahirovic received her doctoral degree (Dr.rer.nat.) from the Center for Molecular Biology of Heidelberg University (ZMBH), and did her post-doctoral training at the Max-Planck-Institute of Neurobiology (MPI) in Munich. Since 2010, Dr. Tahirovic is a group leader at the German Center for Neurodegenerative Diseases (DZNE) in Munich. Her research group integrates primary tissue culture and novel ex vivo models with in vivo, omics and translational approaches to identify molecular fingerprints of microglial dysfunction in Alzheimer´s disease (AD). Recently, Dr. Tahirovic started characterizing microglial pathology in a childhood dementia disorder Niemann Pick type C (NPC) and obtained for this work a Neurodegeneration Research Award from the NCL & Joachim Herz Foundation. Major research goal of her team is to identify novel cellular targets that can “rejuvenate” microglial dysfunction and help in developing therapeutic approaches to monitor and target neuroinflammation. |
| 16:20 - 16:30 | Discussion |
| 16:30 - 16:50 |
Decreased soluble SORLA levels as CSF biomarker of pathogenic SORL1 genetic variants in Alzheimer’s disease patients
Background: An estimated ~2-3% of early-onset Alzheimer’s disease (AD) patients carry a predicted rare damaging variant in the SORL1 gene, which encodes the SORLA receptor protein. Thus far, >500 unique variants have been identified, but to what extent each variant affects SORLA protein function is unclear. SORLA is cleaved at the neuronal membrane into soluble SORLA (sSORLA) and shed into the interstitial fluid, which flows into the cerebrospinal fluid (CSF). Here, the group tested whether the level of sSORLA in the CSF of AD patients reflects the pathogenicity of the SORL1 variant they carry. Methods: sSORLA levels were determined in CSF from patients from the Amsterdam Dementia Cohort (ADC) using: (1) Western Blotting (WB) - 37 AD patients who carried a SORL1 variant with variable predicted pathogenicity; (2) CSF-proteomics in 606 individuals with AD, minor cognitive impairment (MCI) and normal cognition, including carriers of SORL1 variants with varying predicted pathogenicity. Additionally, the group tested whether changes in sSORLA levels in culture-medium of cell lines transfected with constructs encoding SORL1 variants were representative of changes observed in patient-derived CSF. Results: Using WB, sSORLA levels in carriers of predicted likely pathogenic (n=8) and pathogenic (n=5) SORL1 variants were reduced to 48.6%±18.3% (p=6.8x10-3) and 65.6%±32.0%, (p=2.0x10-1) relative to AD patients who carry benign SORL1 variants (n=11). The in vitro cell-based functional assay demonstrated a similar decrease. With CSF-proteomics the group validated that sSORLA levels from carriers of predicted pathogenic variants (n=3) were significantly reduced relative to carriers of the WT allele (n=135); p=3.8x10-7. Discussion: Decreased sSORLA levels in patient-derived CSF or in in vitro cell-based functional assay may serve as a biomarker for damaging SORL1 genetic variants. These results encourage the investment in precise quantification methods of sSORLA levels. 
Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The Netherlands

Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The NetherlandsHenne Holstege is an Associate Professor at the Amsterdam University Medical Center. After she majored in biochemistry at the University of Leiden she did her PhD at the Netherlands Cancer Institute. During this time Dr Holstege was intrigued by the extraordinary case of a Dutch woman who died at age 115 without any symptoms of cognitive decline because this woman proved that cognitive decline is not inevitable. Holstege set up the 100-plus Study, a cohort study of cognitively healthy centenarians to identify protective genetic and biomolecular factors that associate with the escape of cognitive decline. She analyses the data from the centenarians in context of the genetics and biomolecular factors of (early onset) Alzheimer’s Disease; both extremes on the same cognitive spectrum. Therefore, her lab is involved in large international collaborative joint analysis of sequencing data thousands of Alzheimer Disease cases and cognitively healthy controls the collected by European ADES and American ADSP consortia. Holstege and collaborators are currently identifying novel genes associated with the increased or decreased risk of AD. Here, she applies specific focus on the identification of rare pathogenic variants in the SORL1 gene, which next to APOE-e4 allele, is the most common and strongest risk factor of AD. One of her major goals is, therefore, is to implement adequate clinical counselling strategies of SORL1 variant to the carriers and their family members. For this reason, a part of her lab is embedded in the clinic, and involved in counseling genetically predisposed Alzheimer Disease patients. For her work, Holstege was awarded the Alzheimer Research Prize by the Hans und Ilse Breuer Foundation in 2020. For more information see: www.holstegelab.eu. |
| 16:50 - 17:00 | Discussion |
Chair

Professor Maria Grazia Spillantini FMedSci FRS, University of Cambridge, UK

Professor Maria Grazia Spillantini FMedSci FRS, University of Cambridge, UK
Born in Arezzo (Italy), Maria Grazia Spillantini received a Laurea in Biological Sciences from Florence University and a PhD in Molecular Biology from Cambridge University working at the MRC Laboratory of Molecular Biology. In 1996 she moved to the Department of Clinical Neurosciences at Cambridge University, where she was first a Lecturer, then a Reader, and since 2007 Professor of Molecular Neurology. Her interest is on tauopathies and alpha-synucleinopathies. With her collaborators, she identified alpha-synuclein as the component of the filaments that form the Lewy bodies in Parkinson’s disease, dementia with Lewy bodies and the glial inclusions in multiple system atrophy and described one of the first mutations in the MAPT gene causing frontotemporal dementia. She has received several awards, including the Potamkin Prize and the Jay Van Andel award for achievements in Parkinson’s disease, the Thudicum Medal and the European Grand Prix of the French Foundation Recherce Alzheimer. She is a Fellow of the Royal Society, the Academy of Medical Sciences, Clare Hall (Cambridge) and Knight Officer of the Star of Italy.
| 09:00 - 09:20 |
Regulation and function of the LRRK1 and LRRK2 Rab protein kinases
Autosomal dominant mutations that activate the Leucine Rich Repeat Protein Kinase-2 (LRRK2), are associated with familial Parkinson’s disease. Recent work indicates that hyperactivation of LRRK2 results in lysosomal stress and dysfunction which is potentially linked to Parkinson’s. LRRK2 encodes a multidomain protein and phosphorylates a group of Rab GTPases including Rab8A and Rab10 at a conserved Ser/Thr residue located at the centre of the effector binding switch II motif. LRRK2 phosphorylated Rab8A and Rab10 then interact with a group of scaffolding proteins containing an RH2 domain including RILPL1 (RILP-like protein 1). Professor Alessi will provide an update of where we are with understanding how LRRK2 is activated by binding to various Rab proteins and present new understanding of how the LRRK2 phosphorylated Rab proteins recruit new sets of effectors capable of interacting with the lysosome. He will also describe work that his group has done to characterize the specificity of the PPM1H phosphatase that specifically dephosphorylates Rab proteins. Finally, he will also discuss recent work that they have undertaken on the Leucine-rich-repeat-kinase 1 (LRRK1) a homologue LRRK2 that they have shown phosphorylated Rab7A, that is not a substrate for LRRK2. LRRK1 loss of function mutations cause the bone disorder osteosclerotic metaphyseal dysplasia. The group's recent work that reveals that PKC isoforms activate LRRK1 kinase by phosphorylating conserved residues within the GTPase domain. These data suggest that LRRK1 is a key downstream target of PKC isoforms, and thus LRRK1 is this the second kinase to be activated by PKCs after PKD isoforms. DRA is funded by the UK Medical Research Council [grant number MC_UU_12016/2 (D.R.A.)] and Aligning Science across Parkinson's (ASAP) initiative. MJFF administers the grant (ASAP-000463) on behalf of ASAP and itself. 
Professor Dario Alessi FRS, University of Dundee, UK

Professor Dario Alessi FRS, University of Dundee, UKDario is biochemist whose research focuses on unravelling the roles of poorly characterised components which regulate protein phosphorylation or ubiquitylation pathways linked to human disease. He has contributed to our understanding of several disease relevant signal transduction pathways including PDK1 (diabetes and cancer), LKB1 (cancer), WNKs (blood pressure). Much of Dario’s current work is focused on understanding LRRK2 and how mutations in this enzyme cause Parkinson’s disease. In 1997 Dario became a program leader in the MRC Protein Phosphorylation and Ubiquitylation Unit, where he was appointed as its Director in 2012. He also serves as the Director of the Dundee Signal Transduction Therapy Unit, that is a collaboration between scientists at the University of Dundee and pharmaceutical companies. Dario is passionate about the role that biochemical analysis can play in opening up our understanding of human health and disease. Dario Alessi’s publications have accumulated over 9,0000 citations (h-index 145). He has obtained several awards including the Francis Crick Medal and Lecture (2006) and election to the UK Royal Society (2008). Dario obtained a BSc (1988) and PhD (1991) from the University of Birmingham and carried out postdoctoral at the University of Dundee from (1991 to 1996). |
|---|---|
| 09:20 - 09:30 | Discussion |
| 09:30 - 09:50 |
Exploring endocytic dysfunction in neurons and microglia in late onset Alzheimer’s disease
The endocytic pathway is crucial to the normal functioning of neurons and microglia, two cell types that use it in highly specialised ways. Endocytic risk genes for Alzheimer’s include BIN1, the second most significant LOAD risk factor after APOE, PICALM, CD2AP and SORL1. All of these encode proteins that are key to endocytic recycling and clathrin mediated endocytosis (CME). Current evidence suggests endocytic AD single nucleotide polymorphisms generally cause a reduction in gene expression as a whole or, as is the case for PICALM and BIN1, of specific isoforms. The group therefore aims to understand how changes in expression of endocytic risk genes drive disease mechanisms in human neurons and microglia. Their results demonstrate iPSC-derived microglia with reduced PICALM expression have an altered early endosomal compartment with functional consequences for both CME and phagocytosis. In addition, the group has developed a novel endocytic polygenic risk score (PGRS) and selected Alzheimer's patients with high scores to develop novel iPSC lines from. Using this endocytic PGRS confirms that endocytic genetic risk is predominantly driven by mechanisms effecting the early endocytic pathway. 
Dr Natalie Connor-Robson, Dementia Research Institute, Cardiff University, UK

Dr Natalie Connor-Robson, Dementia Research Institute, Cardiff University, UKHaving completed her PhD on the role of the synuclein family in health and disease with Prof Vladimir Buchman, Dr Connor-Robson joined the Oxford Parkinson’s Disease Centre in 2014 as a Career Development Fellow in the group of Prof Richard Wade-Martins. During this time, she worked on understanding the earliest cellular pathogenic events to occur in Parkinson’s Disease using both rodent and iPSC models. Her work highlighted the extensive roles of LRRK2 mutations in the endocytic and autophagic pathways as well as the role of GBA in Parkinson’s. In 2021, Dr Connor-Robson was awarded an Alzheimer’s Research UK Research Fellowship and joined the UK DRI at Cardiff as an Emerging Leader. Her research programme focuses on understanding the role of endocytic risk genes and polygenic risk in the development of Alzheimer’s disease. |
| 09:50 - 10:00 | Discussion |
| 10:00 - 10:20 |
Understanding VPS35 and retromer dysfunction in Parkinson’s Disease
Mutations in the VPS35 gene cause a late-onset, autosomal dominant form of familial Parkinson’s disease (PD). VPS35 plays a well-established role in the retromer complex that mediates the retrograde sorting and recycling of transmembrane cargo proteins from endosomes to the trans-Golgi network or plasma membrane. Within the retromer, VPS35 forms a trimeric cargo-selective complex together with VPS26 and VPS29, that combines with a sorting nexin dimer and additional accessory factors. The molecular basis of familial mutations in VPS35 remain obscure, whereas the interplay between the retromer complex and other PD-linked gene products in common pathological pathways leading to PD remains poorly defined. Here, Professor Moore describes the group's recent efforts in dissecting the molecular and cellular basis of PD-linked mutations in VPS35. He will discuss the development of novel cellular and animal models for exploring the pathogenic effects of VPS35 mutations, including their efforts to clarify whether mutations act via a gain- or loss-of-function mechanism to induce neurodegeneration. In particular, he will discuss potential functional interactions of VPS35 with other PD-linked proteins such as LRRK2, α-synuclein and tau. The group finds that PD-linked VPS35 mutations enhance LRRK2-dependent Rab phosphorylation in the mouse brain that occurs selectively in astrocytes and drives the relocalisation of LRRK2 to lysosomes. The impact of increased LRRK2 substrate phosphorylation on endolysosomal function, autophagy, ciliogenesis, and neurodegeneration in mutant VPS35 rodent models will be discussed. These studies are important for understanding how retromer dysfunction drives neurodegeneration in PD, and for the identification of novel mechanisms that can be exploited for the development of therapeutic strategies to treat PD. 
Professor Darren Moore, Van Andel Research Institute, USA

Professor Darren Moore, Van Andel Research Institute, USADr Darren Moore received an undergraduate degree from the University of East Anglia in 1998 and a PhD in molecular neuroscience from the University of Cambridge in 2001 in the laboratory of Dr Piers Emson. He conducted postdoctoral training with Professor Ted Dawson in the Department of Neurology and Morris K. Udall Parkinson’s Disease Research Center of Excellence at the Johns Hopkins University School of Medicine in Baltimore. Dr Moore joined the faculty at Johns Hopkins in 2005 as an instructor and became assistant professor in 2006. In 2008, Dr Moore moved to the Swiss Federal Institute of Technology (EPFL) in Lausanne as an assistant professor in the Brain Mind Institute. In 2014, Dr Moore joined the faculty at VAI as an associate professor in neurodegenerative science. He subsequently was promoted to professor in 2017 and to chair of the Department of Neurodegenerative Science in 2020. His laboratory is interested in understanding the biology and pathophysiology of gene products associated with inherited Parkinson’s disease. |
| 10:20 - 10:30 | Discussion |
| 10:30 - 11:00 | Coffee |
| 11:00 - 11:10 |
Selected presentation
Dynamics of endosomal trafficking of α-synuclein by the ubiquitin system George Tofaris University of Oxford, UK While defective α-synuclein homeostasis is central to the pathogenesis of Parkinson’s and related diseases, fundamental questions about its intracellular trafficking and degradation remain unresolved. We have developed a complementation assay in living cells that faithfully recapitulates the dynamic ubiquitination of endogenous α-synuclein in neurons. The authors found that de novo ubiquitination of α-synuclein involves the formation of K63-linked ubiquitin chains and identified the critical lysine residues that become ubiquitinated. The autophagic adaptor NBR1 rather than the ESCRT-0 complex binds to ubiquitinated α-synuclein and mediates its entry into endosomes for subsequent lysosomal degradation. Autophagy or the autophagic chaperone Hsc70 are dispensable for this pathway. Antibody generation against diglycine-modified α-synuclein peptides that were identified by mass spectrometry confirmed that endogenous α-synuclein is similarly ubiquitinated in brain and targeted to the lysosome in rat primary and human iPSC-derived neurons. Collectively, these data elucidate the intracellular trafficking of de novo ubiquitinated α-synuclein and provide the tools for investigating the rapidly turned-over fraction of this disease-causing protein. |
| 11:10 - 11:15 | Discussion |
| 11:15 - 11:25 |
Selected presentation
The molecular cell biology jigsaw of Parkinson’s: piecing together the relationship between LRRK2 and VPS35 Katy McCarron, Hannah Elcocks, Michael Clague and Sylvie Urbé University of Liverpool, UK Defects in the endo-lysosomal system and mitochondrial homeostasis are recurring themes across Parkinson’s Disease (PD) related genes. A [D620N] mutation in the retromer component VPS35 has been linked to autosomal dominant PD. This mutation leads to hyperactivation of a second PD gene product, leucine-rich repeat kinase 2 (LRRK2), which can then phosphorylate a subset of Rab family proteins. The authors have generated isogenic hTERT-RPE1 cell lines expressing either wild-type or D260N-mutated VPS35 in an inducible fashion. They have used this model to systematically test for associated properties, previously claimed in the literature; many of which derive from over-expression studies. They confirm the VPS35-dependent activation of LRRK2 under basal conditions and moreover show that this is able to amplify the effect of endosomal membrane stress on LRRK2 activation. |
| 11:25 - 11:30 | Discussion |
| 11:30 - 11:50 |
Autophagy defects in the gut regulate systemic innate immune activation in a Drosophila model of glucocerebrosidase deficiency

Dr Kerri Kinghorn, University College London, UK

Dr Kerri Kinghorn, University College London, UKDr Kerri Kinghorn is a Wellcome Trust Clinical Research Career Development Fellow at the Institute of Healthy Ageing, University College London (UCL) and an Honorary Consultant Neurologist at the National Hospital for Neurology and Neurosurgery. She completed the MB/PhD programme at the University of Cambridge and post-doctoral research at UCL as a Wellcome Clinical Fellow. This was followed by an Academic Clinical Lecturer post in neurology at Kings College London and a Rosetrees UCL Excellence Fellowship. Dr Kinghorn's research group seeks to understand the underlying pathogenic mechanisms of neurodegenerative disorders using the fruit fly Drosophila melanogaster, as well as cellular models of disease. Her research is focused on unravelling the underlying mechanisms linking genes involved in endosomal-lysosomal intracellular trafficking pathways and Parkinson’s disease. Her current works seeks to understand how endo-lysosomal autophagic defects in the gut and associated changes in its microbiome influence brain pathology via gut-brain axis communication.
|
| 11:50 - 12:00 | Discussion |
| 12:00 - 12:20 |
Parkinson’s associated Leucine-Rich Repeat Kinase 2 is activated at lysosomes
Mutations in the Leucine-rich repeat kinase 2 (LRRK2) gene segregate with inherited Parkinson's disease (PD). Pathogenic mutations are concentrated in a central enzymatic region with both GTPase and kinase activities that is surrounded by protein scaffolding domains. All mutations enhance kinase activity as measured either by autophosphorylation or phosphorylation of principally membrane associated small RAB GTPases. When expressed in cells, LRRK2 is largely cytoplasmic and shows only low activity. However, lysosomal damage causes recruitment of LRRK2 to the lysosomal membrane and enhances LRRK2-dependent RAB phosphorylation. Consequently, phosphorylated RABs recruits the motor adaptor protein JIP4, leading ads to extrusion of the lysosomal membrane to form a tubule, a process the group named LYsosomal Tubulation/sorting driven by LRRK2 (LYTL). They have also shown LYTL generates a new vesicle via interaction with the endoplasmic reticulum. Additionally, it is possible to induce activation by directing LRRK2 to membranes using a variety of targeting constructs, irrespective of membrane identity. Furthermore, the adaptor protein JIP4 plays an additional role in controlling this pathway by directing lysosomes towards the perinuclear region of the cell where LYTL is most active. Collectively, these results show that LRRK2 has an essential role in the endolysomal system and are consistent with data in vivo that show that LRRK2 deficiency results in enlarged lysosomes. 
Dr Mark Cookson, NIA, NIH, USA

Dr Mark Cookson, NIA, NIH, USADr Mark R Cookson is a cell biologist whose current research interests include the effects of mutations in the genes associated with neurodegeneration at the cellular and molecular level. His laboratory efforts are directed at finding the underlying pathways that lead to Parkinson's disease and related disorders. Dr Cookson received both his BSc and PhD degrees from the University of Salford, UK in 1991 and 1995, respectively. His postdoctoral studies included time spent at the Medical Research Council laboratories and at the University of Newcastle, UK. He joined the Mayo Clinic, Jacksonville, Florida, as an Assistant Professor in 2000 and moved to the NIA in February 2002. Within the Laboratory of Neurogenetics, Dr Cookson's group works on the effects of mutations associated with Parkinson's disease on protein function. |
| 12:20 - 12:30 | Discussion |
Chair

Professor Sir John Hardy FMedSci FRS, UCL, UK

Professor Sir John Hardy FMedSci FRS, UCL, UK
Following his PhD, Hardy did postdoctoral research at the MRC Neuropathogenesis Unit in Newcastle upon Tyne, England and then further postdoctoral work at the Swedish Brain Bank in Umeå, Sweden where he started to work on Alzheimer's disease. He became Assistant Professor of Biochemistry at St. Mary's Hospital, Imperial College London in 1985 and initiated genetic studies of Alzheimer's disease there, before moving to the USA in 1989 then taking the Pfeiffer Endowed Chair of Alzheimer's Research at the University of South Florida, in Tampa in 1992. In 1996 he moved to Mayo Clinic in Jacksonville, Florida, as Consultant and Professor of Neuroscience. He became Chair of Neuroscience in 2000 and moved to National Institute on Aging, Bethesda, Maryland, as Chief of the Laboratory of Neurogenetics in 2001. In 2007 he took up the Chair of Molecular Biology of Neurological Disease at the Reta Lila Weston Institute of Neurological Studies, University College London. November 2015, he was awarded the Breakthrough Prize 2016 and in 2018 jointly the Brain Prize from The Lundbeck Foundation in Denmark. In 2022 he was awarded a Knighthood in the New Year’s Honours in recognition of contributions to human health and dementia research, and in June 2022 he was conferred as an Honorary Doctor of the University of Helsinki.
| 13:30 - 13:50 |
Common genetic risk for Parkinson’s disease and endolysosomal dysfunction
Dysfunction of the lysosomal system has been strongly implicated in the aetiology of Parkinson’s disease, principally through the identification of rare monogenic variants associated with familial forms of the disorder. Genome wide association studies for Parkinson’s have revealed a complex landscape of common genetic variants linked to heightened risk of disease, with a number of candidate genes connected to endolysosomal cellular functions. Recent research from our group and others has highlighted GPNMB, located on chromosome 7, as a candidate for genome wide significant risk for Parkinson’s at this locus. Using cellular models for GPNMB, the group is investigating connections between GPNMB and lysosomal function, testing for links to other genes with established mechanistic connections to Parkinson’s. 
Professor Patrick Lewis, Royal Veterinary College, UK

Professor Patrick Lewis, Royal Veterinary College, UKPatrick Lewis is an academic at the Royal Veterinary College, University of London. His research centres on the molecular mechanisms of neurodegeneration, with a particular interest in the links between Leucine Rich Repeat Kinase 2 and cellular pathways linked to macroautophagy and lysosomal dysfunction. |
|---|---|
| 13:50 - 14:00 | Discussion |
| 14:00 - 14:10 | Selected presentation |
| 14:10 - 14:15 | Discussion |
| 14:15 - 14:25 |
Selected presentation
Investigating the mechanistic role of STX6 in prion disease and related tauopathies Elizabeth Hill1, Emma Jones1, Juan Ribes1, Melissa Rayner1, Christian Schmidt1, Parvin Ahmed1, George Thirlway1, Azadeh Khalili-Shirazi1, Stephanie Canning1, Tom Cunningham1, Emmanuelle Viré1, John Collinge1 and Simon Mead1 1MRC Prion Unit at UCL, UCL Institute of Prion Diseases,UK Sporadic Creutzfeldt-Jakob disease (sCJD) is the most common human prion disease, occurring when the cellular prion protein (PrPC) spontaneously misfolds into a disease-associated form. Syntaxin-6 (STX6), encoding a SNARE protein involved in early endosome to trans-Golgi network retrograde transport, was recently proposed as a risk gene for sCJD, likely driven by increased STX6 brain expression. The underlying mechanisms could be shared with other neurodegenerative diseases with syntaxin-6 also implicated in progressive supranuclear palsy and Alzheimer’s disease. The aim of this work is to test the hypothesis that increased STX6 expression increases susceptibility to prion diseases and related tauopathies using a functional genetics approach. This work shows that syntaxin-6 colocalises with PrPC in two prion-susceptible cell lines, CAD5 and PK1 neuroblastoma cells. Stable Stx6 knockdown in CAD5 cells, but not PK1 cells, increased prion propagation but PrPC localisation was not consistently altered. Interestingly, STX6 risk variants result in predominant STX6 overexpression in oligodendrocytes raising the potential of non-cell autonomous effects, supporting study of syntaxin-6 in multicellular models. Importantly, prion-infected Stx6-/- mice had extended survival, providing evidence for a pathological role of syntaxin-6 in prion disease. The precise mechanistic role of syntaxin-6 in prion disease and tauopathies are subjects of ongoing research. Acknowledgments: Fahri Küçükali and Julien Bryois for data and idea sharing. MRC Harwell for the generation of the Stx6 -/- mice and our animal facility for animal care. |
| 14:25 - 14:30 | Discussion |
| 14:30 - 14:50 |
VPS35 causal mutations in Parkinson’s disease
VPS35 was identified as a causative gene for Parkinson’s disease (PD) by massive parallel sequencing in large multi-incident families. To date, only one mutation is widely considered pathogenic: p.Asp620Asn (p.D620N, c.1858G>A). According to the MDSGene database, a total of ten different sequence variants were reported in the VPS35 gene and were mostly missense (90%). Besides the definitely pathogenic variant, two were classified as probably pathogenic and seven as possibly pathogenic. Of the 67 carriers of heterozygous VPS35 variants, 50 (75%) carried the definitely pathogenic p.D620N variant, four (6%) a probably, and 13 (19%) a possibly pathogenic variant. The 67 VPS35 mutation carriers originated from 41 families, with 34% being men. Their clinical presentation is practically indistinguishable from that of idiopathic PD patients, except for a slightly earlier age of onset of a median of 52 years (range: 26-75 years). The ethnicity of families is White, Asian, and Ashkenazi Jewish (45%, 35%, and 20%, respectively). Most of the identified families originated from Austria (38%), France/Switzerland (13-15%), or the USA (10%). PARK-VPS35 patients respond well to L-Dopa treatment; non-motor signs are reported at similar frequencies as in idiopathic PD. Unpublished data from the Michael J Fox Foundation Global Monogenic Parkinson’s Disease Project revealed 26 carriers of VPS35 pathogenic variants, including three unaffected ones confirming the reduced penetrance of VPS35 pathogenic variants. However, the extent of the reduced penetrance cannot yet be determined with certainty due to the overall small sample size of reported variant carriers. Recent data from the independent ROPAD study performing panel sequencing of PD genes in 1,360 PD patients revealed two carriers of the p.D620N variant, underscoring the overall rarity of this variant in PD. As a future perspective, ~150,000 individuals (patients and controls) will be tested for the p.D620N variant within the Global Parkinson’s Genetics Program over the coming three years. This large-scale, multi-ethnic project will result in more profound insights into the frequency and phenotypic spectrum of VPS35 variant carriers in different populations, determine the penetrance of this variant, and may lay the ground for genetic modifier studies of penetrance and age at onset. 
Professor Christine Klein, University of Lübeck, Germany

Professor Christine Klein, University of Lübeck, GermanyDr. Christine Klein is a Professor of Neurology and Neurogenetics. She studied medicine in Hamburg, Heidelberg, Luebeck, London, and Oxford (UK) and did internships in Stockholm (Sweden), Rennes (France), Wollongong (Australia) and Vitebsk (Belarus). She moved to Boston from 1997-1999 for a fellowship in Molecular Neurogenetics with Dr. X.O. Breakefield and completed her neurology training at Luebeck University in 2004, followed by a series of summer sabbaticals in movement disorders with Dr. A.E. Lang in Toronto, Canada in 2004-2015. She was appointed Lichtenberg Professor at the Department of Neurology of Luebeck University in 2005, where her research has focused on the clinical and molecular genetics of movement disorders and its functional consequences. In 2009, Dr. Klein was appointed Schilling Professor of Clinical and Molecular Neurogenetics at the University of Luebeck and became Director of the newly founded Institute of Neurogenetics in 2013. Dr. Klein has published >500 scientific papers and has an h-factor of 100 with >42,000 citations. She is Deputy Editor of ‘Movement Disorders’ and ‘Science Advances’ and former Associate Editor of ‘Annals of Neurology’ (until 2021), served as chair of the Congress Scientific Program Committee of the 2016/2017 Annual Congresses of the International Parkinson and Movement Disorder Society, is the acting Past-President of the German Neurological Society (~11,000 members) and Chair-elect of the European Section of the International Parkinson and Movement Disorder Society (MDS-ES). She has been elected a member of the National Academy of Sciences Leopoldina in 2021. Ten of her former doctoral students or mentees have been promoted to the level of assistant, associate, or full professor. |
| 14:50 - 15:00 | Discussion |
| 15:00 - 15:20 |
Talk title tbc

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, Canada

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, CanadaPeter St George-Hyslop FRS is a medical scientist, neurologist and molecular geneticist who is distinguished for his research into neurodegenerative disorders, including Alzheimer’s disease (AD). In particular, he discovered several genes that when mutated lead to early onset hereditary AD, accelerating our understanding the disease and the development of potential treatments. His discovery that defective genes encoding presenilins are a cause of familial AD led to presenilins becoming a new target for treatments. He went on to show that mutated presenilins contribute to the generation of the amyloid beta protein — deposition of which is the earliest sign of AD in those carrying such genes. His work on several other neurodegeneration-related genes and proteins (including SORLA, TREM2, FUS and ANXA11) has led to an understanding of the role of vesicular transport, inflammation and perturbed RNA granule biology. Peter has led an AD research programme as Professor of Experimental Neuroscience at the University of Cambridge since 2007. He was awarded the Howard Hughes Medical Institute International Scholar Award in both 1997 and 2002, and has received several other notable awards. |
| 15:20 - 15:30 | Discussion |
| 15:30 - 16:00 | Tea |
| 16:00 - 17:00 |
Panel discussion

Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The Netherlands

Dr Henne Holstege, Clinical Genetics and Alzheimer Center Amsterdam UMC, The NetherlandsHenne Holstege is an Associate Professor at the Amsterdam University Medical Center. After she majored in biochemistry at the University of Leiden she did her PhD at the Netherlands Cancer Institute. During this time Dr Holstege was intrigued by the extraordinary case of a Dutch woman who died at age 115 without any symptoms of cognitive decline because this woman proved that cognitive decline is not inevitable. Holstege set up the 100-plus Study, a cohort study of cognitively healthy centenarians to identify protective genetic and biomolecular factors that associate with the escape of cognitive decline. She analyses the data from the centenarians in context of the genetics and biomolecular factors of (early onset) Alzheimer’s Disease; both extremes on the same cognitive spectrum. Therefore, her lab is involved in large international collaborative joint analysis of sequencing data thousands of Alzheimer Disease cases and cognitively healthy controls the collected by European ADES and American ADSP consortia. Holstege and collaborators are currently identifying novel genes associated with the increased or decreased risk of AD. Here, she applies specific focus on the identification of rare pathogenic variants in the SORL1 gene, which next to APOE-e4 allele, is the most common and strongest risk factor of AD. One of her major goals is, therefore, is to implement adequate clinical counselling strategies of SORL1 variant to the carriers and their family members. For this reason, a part of her lab is embedded in the clinic, and involved in counseling genetically predisposed Alzheimer Disease patients. For her work, Holstege was awarded the Alzheimer Research Prize by the Hans und Ilse Breuer Foundation in 2020. For more information see: www.holstegelab.eu. 
Professor Peter Cullen, University of Bristol, UK

Professor Peter Cullen, University of Bristol, UKBiography not available 
Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, Canada

Professor Peter St George-Hyslop FRS, Cambridge Institute for Medical Research, UK and University of Toronto, CanadaPeter St George-Hyslop FRS is a medical scientist, neurologist and molecular geneticist who is distinguished for his research into neurodegenerative disorders, including Alzheimer’s disease (AD). In particular, he discovered several genes that when mutated lead to early onset hereditary AD, accelerating our understanding the disease and the development of potential treatments. His discovery that defective genes encoding presenilins are a cause of familial AD led to presenilins becoming a new target for treatments. He went on to show that mutated presenilins contribute to the generation of the amyloid beta protein — deposition of which is the earliest sign of AD in those carrying such genes. His work on several other neurodegeneration-related genes and proteins (including SORLA, TREM2, FUS and ANXA11) has led to an understanding of the role of vesicular transport, inflammation and perturbed RNA granule biology. Peter has led an AD research programme as Professor of Experimental Neuroscience at the University of Cambridge since 2007. He was awarded the Howard Hughes Medical Institute International Scholar Award in both 1997 and 2002, and has received several other notable awards. 
Professor Scott Small, Columbia University, USA
Professor Scott Small, Columbia University, USAScott A. Small MD is the Director of the Alzheimer’s Disease Research Center at Columbia University, where he also directs the Psychosis Research Program. Dr. Small focuses on disorders that affect the hippocampus, a brain structure targeted by Alzheimer’s disease, schizophrenia, and the normal wear & tear of the aging process. The hippocampus is a circuit comprised of a handful of microscopic regions. The overarching hypothesis motivating Dr. Small’s lab is that if hippocampal regions most vulnerable to a disorder can be pinpointed, this anatomical information can guide a search for the disorder’s root cause. Accordingly, Dr. Small’s ‘anatomical biology’ lab has pioneered the development of MRI tools best suited to isolate vulnerable hippocampal regions. His lab has then used this information to identify mechanisms that are now thought to underlie Alzheimer’s disease, schizophrenia, and ‘cognitive aging’. Most recently, his lab has begun developing interventions for each condition. To date, the lab has completed two clinical trials for cognitive aging and one for schizophrenia, and the lab’s Alzheimer’s disease findings was the cornerstone around which a new biotechnology company, Retromer Therapeutics. was formed. |
