Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Reducing neonatal infectious morbidity and mortality: joining up our thinking
Theo Murphy scientific meeting organised by Dr Kirsty Le Doare, Dr Elizabeth Whittaker, Professor Beate Kampmann and Dr Chrissie Jones.
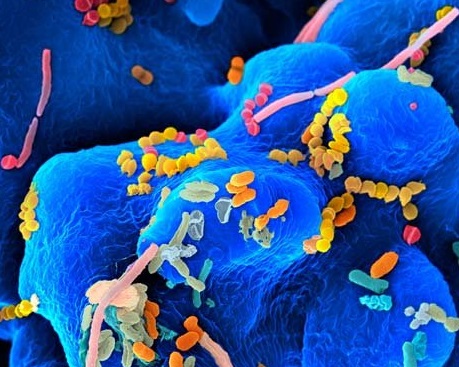
Whilst under-5 mortality has declined globally, neonatal mortality remains static, largely due to infection. Understanding how neonatal immune responses differ to adults will aid development of targeted neonatal infection prevention and management strategies. This meeting will discuss recent scientific advances and propose a research agenda for collaborative international research to reduce the burden of community and hospital-acquired neonatal infection.
The schedule of talks, speaker biographies and abstracts are available below. Recorded audio of the presentations are also available below.
Attending this event
This is a residential conference, which allows for increased discussion and networking.
- Free to attend
- Advanced registration essential
- Catering and accommodation available to purchase during registration
Enquiries: Contact the Scientific Programmes team
Organisers
Schedule
Chair

Dr Chrissie Jones, St George's, University of London, UK

Dr Chrissie Jones, St George's, University of London, UK
Dr Chrissie Jones is an Associate Professor in Paediatric Infectious Diseases at the University of Southampton. Her research interests include interventions in pregnancy to prevent infection in early life. She has particular expertise in the field of maternal vaccination and leads pertussis and RSV clinical trials in pregnancy. She serves on the executive committee of GAIA (http://gaia-consortium.net), a large international consortium. As part of this initiative, Dr Jones has authored international guidelines to provide a standard for data collection in clinical trials of vaccines in pregnancy, which are recommended by the WHO.
Dr Jones is the chief investigator of RACE-FIT, a NIHR-funded feasibility study to assess an educational intervention to reduce the risk of CMV acquisition in pregnancy.
With postgraduate training in medical education, Dr Jones is involved with multiple initiatives to train and equip others in paediatric infectious diseases.
| 09:05 - 09:25 |
5.7 million neonatal deaths and stillbirths: infections, organisms and measurement black holes
Of the annual 2.7 million neonatal deaths, the most recent estimates for 196 countries suggest that neonatal infections causes approximately 600,000 deaths, almost double the number of child deaths from malaria plus HIV/AIDS. Yet for neonatal infections (apart from tetanus) there is much slower mortality reduction, and very limited global health investment. If the closely linked burden of 2.6 million stillbirths could be accurately assessed for infection, and the impairment outcomes for survivors of neonatal infection were included then the associated burden would be even more striking. There are measurement black holes which impede evidence based investment and faster reduction of this burden, but could be targeted. For example, new analysis shows the important contribution of group B streptococcus to stillbirths, as well as neonatal invasive disease, with implications for cost-effectiveness of maternal vaccination. Some of the most important measurement black holes regarding neonatal infections will be detailed, highlighting opportunities for change, notably the following: aetiological data, stillbirth investigations including infection aetiology, impairment outcomes for survivors of neonatal infections, and measuring the coverage and quality of care.

Professor Joy Lawn FMedSci, London School of Hygiene & Tropical Medicine, UK

Professor Joy Lawn FMedSci, London School of Hygiene & Tropical Medicine, UKJoy is an African-born, British-trained paediatrician and perinatal epidemiologist with 25 years of experience including clinical care, epidemiological burden estimates, and the design and evaluation of integrated maternal, newborn and child care services at scale, especially in sub-Saharan Africa. Her medical degree and paediatric training were in the UK, followed by teaching, programme and research work, mainly in Africa, including a decade with Saving Newborn Lives/Save the Children. Her MPH was at Emory, Atlanta, USA, whilst working at CDC, and her PhD was through Institute of Child Health London. Joy’s particular contribution has been in developing the evidence-base for policy and programming change to measure and address the global burden of 2.7 million neonatal deaths, 2.7 million third trimester stillbirths, and 15 million preterm births. This work came to prominence through Lancet Neonatal Survival series (2005), Lancet Stillbirth series in 2011 and 2016, and especially the Lancet Every Newborn series (2014) with the associated Every Newborn Action Plan, endorsed at the World Health Assembly and supported by >80 partners. She co-chairs the UN’s Every Newborn metrics work to increase the quantity, quality and use of data. She has published <150 peer reviewed papers, with an H index of over 80, as well as several widely used policy relevant reports, launched with major media attention, and a number of academic chapters. She is currently professor of Epidemiology, at the London School of Hygiene & Tropical Medicine and Director of Maternal, Adolescent, Reproductive & Child Health (MARCH) centre including 200 academics from multiple disciplines organised around three research themes: Adolescents, Births, and Child health and development. She leads a research team of more than 20 scientists working on newborn health, stillbirths and child development around the world. She is the School’s Aurora Women’s Leadership Champion. Joy has been awarded a number of prestigious prizes such as the Nils Rosen von Rosenstein medal for paediatrics, PGPR Global Child Health award, Wolfson Royal Society Merit award and Fellowship of Academy of Medical Sciences. |
|
|---|---|---|
| 09:40 - 10:00 |
Gram-negative bacterial infections in the neonate – global epidemiology
Gram-negative bacterial infections, in particular sepsis caused by Gram-negative bacteria, can have devastating consequences during the neonatal period. Rising levels of antimicrobial resistance among Gram-negative bacteria globally are an additional cause for concern, as therapeutic options are limited. In particular, data from lower and middle income countries, where neonates experience a high burden of infections with considerable associated mortality and morbidity, demonstrate that many Gram negative isolates are resistant to both first- and second-line empiric regimens recommended by the World Health Organization. Furthermore, there are a number of reports of outbreaks caused by multidrug resistant Gram-negative bacteria in the setting of neonatal inpatient care. It has been estimated that up to 30% of neonatal deaths due to sepsis are attributable to multi-drug resistant bacteria, with extended-spectrum beta-lactamase producing Gram negative bacteria being among the main culprits. However, available surveillance data is of insufficient quality to gain robust insights into the global epidemiology of neonatal Gram-negative bacterial infections. Improved and integrated surveillance is necessary to identify the areas of greatest therapeutic need in this population. Currently available antibiotic treatment options are limited, and the potential effectiveness of other interventions has not been sufficiently studied. Alternative interventions range from non-invasive attempts to influence the colonising microflora (for example through increased mother-baby skin-to-skin contact) to the prophylactic use of monoclonal antibodies against key bacteria. 
Dr Julia Bielicki, St George's, University of London, UK

Dr Julia Bielicki, St George's, University of London, UKJulia Anna Bielicki is a Senior Researcher in Paediatric Infectious Disease at St George’s University of London. Julia trained in paediatrics and infectious diseases at the Evelina Children’s Hospital and St Mary’s Hospital, London, as well as in Zurich and Basel, Switzerland and in 2011 obtained a Master of Public Health degree from the London School of Hygiene and Tropical Medicine. Julia’s particular research interests are in observational and interventional studies that aim to improve antibiotic use for neonates and children in the light of an increasing burden of antimicrobial resistance and the need to conserve antibiotics for future generations. From 2011 to 2014, Julia co-ordinated the Antibiotic Resistance and Prescribing in European Children (ARPEC) Project, which recruited nearly 20’000 children from over 40 countries worldwide. Building on this, she will be leading a multi-national prospective observational cohort of neonatal sepsis and bloodstream infection as part of a new programme of work focusing on the impact of antimicrobial resistance on management of neonatal infection in lower and middle income countries. |
|
| 10:50 - 11:10 |
Group B Streptococcal disease and neonatal susceptibility to infection
Neonatal group B streptococcal sepsis is a highly inflammatory disease, where bacterial effectors induce cytokines leading to end organ failure, long term sequels and lethality. We have identified the interaction of streptococcal RNA and lipopeptides with Toll-like receptors and cytosolic sensors as key molecular events in this process. Moreover, tissue specific changes in immune cell composition under influence of the emerging microbiota substantially contribute to susceptibility to infection and course of the disease. Accordingly, manipulation of the site specific innate immune cell response on the cognate receptor level is a rational strategy for improving outcome in group B streptococcal sepsis. 
Professor Philipp Henneke, Center for Pediatrics and Center for Chronic Immunodeficiency, University of Freiburg, Germany

Professor Philipp Henneke, Center for Pediatrics and Center for Chronic Immunodeficiency, University of Freiburg, GermanyPhilipp Henneke is Professor of Infection and Immunity and Head of the Division of Paediatric Infectious Diseases and Rheumatology at the Centre for Paediatrics and Adolescent Medicine (Medical Centre, University of Freiburg). He is Principal Investigator of a research and diagnostic laboratory, which focuses on antimicrobial phagocyte biology and innate immunity. After graduating from Freie Universität Berlin, he received basic training in paediatrics and infectious diseases at the Children’s Hospital, Freie Universität Berlin. Subsequently, he worked as a Lecturer at Harvard Medical School, Boston and as an Assistant Professor at the University of Massachusetts Medical School. In 2003, he joined the Faculty of Medicine, Freiburg, as an Assistant Professor in Paediatric Infectious Diseases. Since then he has been appointed Full Professor. Philipp Henneke has received several scientific awards, such as the ‘Young Investigator Award’ of the European Society for Paediatric Infectious Diseases, the ‘Hugo-Schottmüller-Award’ by the German Sepsis Society and the ‘Science Award’ by the German Society for Paediatric Infectious Diseases (DGPI). Currently he is editor of the Journal of Pediatric Infectious Diseases, Board Member of the German society for paediatric infectious disease (DGPI) and Head of the Research Committee of the ESPID (European Society of Paediatric Infectious Diseases). Philipp Henneke’s scientific area of interest is the development of foetal/neonatal innate immunity, molecular mechanisms in receptor mediated innate immunity to Gram-positive bacteria, immunodeficiency to bacterial infections, and novel translational approaches to adjuvant sepsis therapy. His clinical specialities are bacterial sepsis, and mycobacterial infections and congenital infections. |
|
| 11:30 - 11:50 |
Global burden of congenital CMV infection
Cytomegalovirus (CMV) is a leading cause of congenital infection worldwide. In the developed world, it is a leading non-genetic cause of childhood hearing loss and neurodevelopmental disabilities. The prevalence of congenital CMV infection is directly related to CMV seroprevalence in women of child-bearing age. Therefore, the populations in the developing world experience the higher prevalence of congenital CMV infection (1-5% of births) and are most likely driven by non-primary maternal infections. Although reliable estimates of prevalence and outcome from different regions of the world are not available, recent data demonstrating similar rates of hearing loss following primary and non-primary maternal infection have underscored the importance of congenital CMV infection in resource-poor settings. Therefore, successful implementation of strategies to prevent or reduce the burden of congenital CMV infection will require heightened global awareness among clinicians and the general population and a better understanding of the factors associated with intrauterine transmission of CMV following non-primary maternal infections. This talk will highlight the global epidemiology of congenital CMV with particular emphasis on the disease burden in resource-poor settings. 
Professor Suresh Boppana, University of Alabama School of Medicine, USA

Professor Suresh Boppana, University of Alabama School of Medicine, USADr Suresh Boppana is a Professor of Pediatrics and Microbiology at the University of Alabama at Birmingham and directed the UAB Pediatric Infectious Diseases Training Program for 10 years. He has been studying the natural history and pathogenesis of maternal and congenital cytomegalovirus (CMV) infection. His research interests include the mechanisms of intrauterine transmission of CMV, global burden and pathogenesis of congenital CMV infection, and the consequences of CMV reinfections. His work challenged the dogma that most of the disease burden from congenital CMV infection is seen in children born to women with primary CMV infection during pregnancy and documented the impact of congenital CMV resource-limited settings with high seroprevalence. He showed that CMV reinfections occur frequently and can lead to intrauterine infection, symptomatic disease and sequelae. As the PI of a large multicentre study newborn CMV screening study supported by NIH, his group defined the contribution of congenital CMV infection to childhood deafness and developed a real-time PCR assay that has been shown to be highly sensitive and specific to detect CMV in newborn saliva specimens and can be adapted for newborn CMV screening. He mentored numerous trainees and served as a member NIH review committees. Dr Boppana is a Fellow of the American Academy of Pediatrics and Infectious Diseases Society of America, and an active member of the Pediatric Infectious Diseases Society and the American Society for Microbiology. |
|
| 12:10 - 12:35 |
Neonatal innate immunity to RSV: from pathogenesis to protection
Respiratory syncytial virus (RSV) is the leading cause of infant lower respiratory tract infection, accounting for 33.8 million episodes of acute respiratory tract infection and 66,000 – 199,000 deaths annually. Over 80% of severe RSV infections occur in otherwise healthy neonates and infants <6 months, urging for novel strategies to protect this vulnerable age group. Toll-like receptor (TLR) responses play an essential role in the defence against RSV. Efficient viral clearance requires pathogen recognition through TLR4 and induction of a Th1-type immune response. In contrast, severe RSV disease is characterised by a Th2-type immune response, characterised by low levels of pro-inflammatory cytokines and high levels of IL-10. The distinct function of the neonatal TLR system, which is intrinsically biased against production of pro-inflammatory responses and favours production of IL-10, may predispose to severe RSV infection. This is supported by recent studies, which show that age-dependent differences in dendritic cells shape the immune response to RSV, and that neonatal dendritic cells require more co-stimulation than adult dendritic cells to induce protective responses. The early postnatal period is essential for the development of the neonatal TLR system, and may provide a unique window of opportunity to prevent subsequent RSV bronchiolitis. For instance, environmental factors, such as breast feeding, presence of siblings and mode of delivery, have been shown to modulate postnatal TLR maturation. In addition, mechanistic studies have identified neonatal blood plasma as an important source of immune modulatory factors, which may provide novel targets to modulate neonatal innate responses and to optimise antiviral immunity. This talk will discuss how insights into the neonatal innate immune system can be exploited to reduce the global burden of RSV infection. 
Dr Mirjam Belderbos, University Medical Center Groningen, The Netherlands

Dr Mirjam Belderbos, University Medical Center Groningen, The NetherlandsDr Mirjam Belderbos is a paediatrician and clinician scientist. Her main interests include how immune impairments contribute to disease, such as infections, asthma and cancer, and how the immune system can be exploited to prevent and/or treat disease. This applies to known immune deficiency syndromes, but also to situations of ‘physiological’ immune tolerance, such as pregnancy and neonates. Dr Belderbos obtained a PhD in immunology in 2011 (Professor Bont and Professor Meyaard, UMC Utrecht). Her thesis focuses on the neonatal innate immune system in the pathogenesis of Respiratory Syncytial Virus (RSV) bronchiolitis. Dr Belderbos’ work demonstrates that the first month of life is essential for the development of the innate immune system, during which neonatal Toll-like receptor responses shift from tolerant (Th2-polarised) responses to a more pro-inflammatory (Th1-polarised) phenotype. In collaboration with the group of Professor Ofer Levy, Harvard Medical School, she demonstrated that soluble mediators in neonatal plasma contribute to impaired neonatal innate immunity. After finishing her PhD studies, Dr Belderbos moved to Groningen, where she combined her clinical training in paediatrics with a postdoctoral fellowship in Stem Cell Biology at the European Research Institute for the Biology of Ageing. Her work was awarded various personal and career grants. She is a reviewer for several journals in paediatrics, immunology and oncology. She is a member of the Dutch Cancer Society, the International Society of Experimental Hematology and the Dutch Society for Pediatrics. |
Chair

Dr Elizabeth Whittaker, Imperial College London, UK

Dr Elizabeth Whittaker, Imperial College London, UK
Doctor Elizabeth Whittaker is an Academic Clinical Lecturer in Paediatric Infectious Diseases and Immunology at Imperial College London. Her main research interests are age-related immune responses to infectious diseases, in particular infants under a year of age. She completed her undergraduate training in medicine at Trinity College, Dublin, Ireland, including an HRB (Health Research Board) funded BSc in Immunology. Following this she trained as a paediatrician in London and was successfully awarded an Academic Clinical Fellowship in Paediatric Infectious diseases. She completed her Wellcome Trust funded PhD ‘Age-related immune responses to Mycobacteria’ in the laboratories of Professor Beate Kampmann at Imperial College and Professors Mark Nicol and Heather Zar at the University of Cape Town. She divides her time between clinical work, research and teaching, and practising as a paediatric Consultant at St. Marys Hospital, London.
| 13:30 - 14:00 |
The impact of maternal infections in pregnancy on the neonatal immune system
Epidemiological studies suggest that chronic infections during pregnancy impact the susceptibility of young children to homologous or heterologous pathogens. This impact probably involves multiple factors but maternal programming of the neonatal immune system is likely to be involved. The implementation of anti-retroviral therapy during pregnancy has markedly increased the number of HIV-exposed but uninfected (HEU) infants. Studies from low- and high-income countries indicated that HEU infants are at high risk of severe infections caused by a variety of pathogens. Immune abnormalities, including the decreased transfer of maternal antibodies and activation of the newborn immune system, as well as haematological toxicity of anti-retrovial therapy (ARVT) have been proposed as possible mechanisms. In a prospective birth cohort study conducted in Belgium, HEU infants had a two-fold higher risk of hospitalisation for infection as compared to HIV-unexposed infants. The results of this study will be presented and the identification of immunological biomarkers associated with severe infections will be discussed. 
Dr Arnaud Marchant, Institute for Medical Immunology, Université Libre de Bruxelles, Belgium

Dr Arnaud Marchant, Institute for Medical Immunology, Université Libre de Bruxelles, BelgiumArnaud Marchant MD PhD is currently based at the Université Libre de Bruxelles, Belgium. His research activities include the study of immune responses to viral infections and vaccines in humans and the ontogeny of the human immune system. He developed a research programme in infant immunology during a post-doctoral stay at the Medical Resarch Council Laboratories, The Gambia that he pursued at the Weatherall Institute for Molecular Medicine, Oxford. He is currently a senior research associate at the Fund for Scientific Research, Belgium and he is the director of the Institute for Medical Immunology of the Université Libre de Bruxelles. Arnaud Marchant teaches medical immunology at the medical faculty of the Université Libre de Bruxelles. |
|---|---|
| 14:15 - 14:45 |
Susceptibility to infectious disease in the newborn
Neonatal infection causes nearly 1 million deaths per year. This horrific clinical reality is often ascribed to a lower capacity of the newborn immune system to fend off invading microbes. However, there also is substantial evidence for an exuberant host immune response to infection in the newborn. This apparent contradiction (lower vs. higher immune activity) indicates that the often-used explanation (‘the newborn immune systems is less capable, i.e. immature’) does not capture this complex reality. The paradigm implicating age-specific regulatory adaptations rather than simply lower effector mechanisms for an increase in morbidity and mortality in early life fits the existing data much better. Specifically, the particular demands in early life demand maintenance of tolerance and balancing of pro-inflammatory stimuli. As a result, the threshold required to initiate immune effector responses is appropriately set higher in early vs. later life. However, once this higher set point is reached, an immune response of substantial magnitude is unleashed that can lead to higher immune pathology. In this context, the clinically observed increased risk for severe infection in early life is best viewed as an imbalance of the phylogenetically selected beneficial survival programs vs. specific environmental demands exerted on the individual during ontogeny. It follows that increased protection from infectious diseases in early life could benefit from an increase of homeostatic stimuli and a decrease rather than increase of immune effector responses. 
Professor Tobias Kollmann, University of British Columbia, Canada

Professor Tobias Kollmann, University of British Columbia, CanadaDr Kollmann completed his MD and PhD at the Albert of Einstein College of Medicine, Bronx NY, followed by a residency in paediatrics and fellowship in infectious diseases at the University of Washington, Seattle, WA. He now is consulting physician in paediatric infectious disease at BC Children’s Hospital, where he directs the training programme in Global Pediatric Infectious Diseases (GpID) and the Vancouver Immune and Vaccine Analysis Research Center (VIVArc). Dr Kollmann focuses on the development of the immune system, with a special focus on infections and vaccines for early life. |
Chair

Professor Beate Kampmann, Imperial College London, UK and MRC Unit The Gambia

Professor Beate Kampmann, Imperial College London, UK and MRC Unit The Gambia
Professor Beate Kampmann holds a Chair in Paediatric Infection & Immunity at Imperial College, London and was appointed as the Scientific Director (Theme Leader) for Vaccinology research at the MRC Unit-The Gambia in July 2010. She leads a comprehensive childhood infection research program both in the UK and sub-saharan Africa, where she spends a third of her time. She has extensive practical and research experience in childhood infection for over 15 years and brings an established funding track record as PI and co-applicant from major international funders for the conduct of laboratory-based and programmatic research in TB and Vaccinology in both resource-poor and resource rich settings. At the MRC Unit in The Gambia, she directs all research activity in infant immunology, ranging from basic research of innate and acquired immune responses to infection and vaccination to clinical trials of novel vaccines and their adjuvants.

Dr Kirsty Le Doare, Imperial College London, UK

Dr Kirsty Le Doare, Imperial College London, UK
Dr Kirsty Le Doare is a consultant in paediatric infection and immunology at Evelina London Children’s Hospital and a Wellcome Trust Fellow at Imperial College London. Her main research interests are age-related immune responses to infectious diseases, in particular to Group B-streptococcus in neonates.
Kirsty is a late starter to medicine, having spent ten years working as an economist for NGOs such as Oxfam, following completion of a joint BA (Hons.) degree/Diplom-Betriebswirtin in European Economic Studies as part of an ERASMUS link between universities in the UK, Germany, Spain and France. Her experience in developing countries led her to enter post-graduate medical training at St. George's University of London. She was successfully awarded an Academic Specialty Training in International Child Health in 2008. She was awarded a prestigious sub-specialty training post in Paediatric Immunology and Infectious Diseases in 2012, the Oxford Masters in Paediatric Infectious Diseases in 2014 and now works as a clinical academic between the Evelina Children’s Hospital, Imperial College London and MRC The Gambia.
Kirsty is currently leading an international collaboration to standardise assays to measure antibody against Group B Streptococcus with the aim of facilitating the development of an immune correlate of protection against GBS colonisation and disease.
Kirsty is a member of the Royal College of Paediatrics and Child Health (MRCPCH), Academic Paediatrics Association (APA), British Paediatric Allergy Infection and Immunity Group (BPAIIG), Children's HIV Association (CHIVA) and International Child Health Group.
| 15:30 - 16:30 | Breakout session: What are the areas of neonatal immunity that we need to increase our understanding of as research priorities and how can we do this? |
|---|---|
| 15:30 - 16:30 | Breakout session: What are the areas of maternal immunity that we need to focus on as research priorities and thoughts on how to do this? |
| 16:30 - 17:00 | Discussion and feedback from sessions |
Chair

Dr Kirsty Le Doare, Imperial College London, UK

Dr Kirsty Le Doare, Imperial College London, UK
Dr Kirsty Le Doare is a consultant in paediatric infection and immunology at Evelina London Children’s Hospital and a Wellcome Trust Fellow at Imperial College London. Her main research interests are age-related immune responses to infectious diseases, in particular to Group B-streptococcus in neonates.
Kirsty is a late starter to medicine, having spent ten years working as an economist for NGOs such as Oxfam, following completion of a joint BA (Hons.) degree/Diplom-Betriebswirtin in European Economic Studies as part of an ERASMUS link between universities in the UK, Germany, Spain and France. Her experience in developing countries led her to enter post-graduate medical training at St. George's University of London. She was successfully awarded an Academic Specialty Training in International Child Health in 2008. She was awarded a prestigious sub-specialty training post in Paediatric Immunology and Infectious Diseases in 2012, the Oxford Masters in Paediatric Infectious Diseases in 2014 and now works as a clinical academic between the Evelina Children’s Hospital, Imperial College London and MRC The Gambia.
Kirsty is currently leading an international collaboration to standardise assays to measure antibody against Group B Streptococcus with the aim of facilitating the development of an immune correlate of protection against GBS colonisation and disease.
Kirsty is a member of the Royal College of Paediatrics and Child Health (MRCPCH), Academic Paediatrics Association (APA), British Paediatric Allergy Infection and Immunity Group (BPAIIG), Children's HIV Association (CHIVA) and International Child Health Group.
| 09:00 - 09:30 |
Age-specific adjuvants for precision vaccines
Vaccines are the most effective biomedical intervention to reduce the heavy burden of early life infection, but often demonstrate suboptimal immunogenicity in early life necessitating multiple boosting doses. Waning immunity to some infant vaccines further limits their effectiveness. Approaches to enhance early life immune responses include identification of adjuvants that increase vaccine immunogenicity. As adjuvants engage innate immune pathways that are often species- and age-specific, the Levy Lab has developed a range of human neonatal and adult in vitro assay platforms to model innate and adaptive immune responses. Human in vitro modelling has identified adjuvants and adjuvant combinations active towards newborn and infant antigen-presenting cells in vitro and that enhance immunogenicity of vaccinal antigens in newborn animals in vivo. Overall, technical advances including human in vitro modelling, genetics and systems biology are ushering in a new era in which precision medicine is brought to vaccinology. In this context, Levy and colleagues recently established the Precision Vaccines Program, a platform for international collaboration to develop vaccines targeted to vulnerable populations such as the very young. 
Dr Ofer Levy, Boston Children's Hospital and Harvard Medical School, USA

Dr Ofer Levy, Boston Children's Hospital and Harvard Medical School, USADr Ofer Levy was born to and raised by the artist Benjamin Levy and music composer Hannah Levy in New York City, where he graduated from the Bronx High School of Science. After graduating from Yale College (B.S., Molecular Biophysics and Biochemistry), Dr Levy entered the Medical Scientist (MD/PhD) Training Program at New York University School of Medicine. There he earned his PhD under the mentorship of Drs Peter Elsbach and Jerrold Weiss, characterising neutrophil-derived antimicrobial proteins and peptides including bactericidal/permeability-increasing protein (BPI) and cathelicidins. Inspired by his wife Sharon’s example, he chose Paediatrics and completed both residency and fellowship (Infectious Diseases) at Boston Children’s Hospital. He is currently Associate Professor at Harvard Medical School as well as principal investigator, staff physician and the Director of the Precisions Vaccine Program in the Division of Infectious Diseases, Boston Children’s Hospital. Dr Levy’s laboratory is focused on modelling vaccine-induced human immune responses in vitro using a variety of platforms including three-dimensional microphysiologic systems as well as global molecular (‘OMIC’) approaches to accelerate and de-risk development of vaccines optimised for populations with distinct immune responses, including those at the extremes of age who suffer the most infections. He currently leads an NIH/NIAID Adjuvant Discovery Program contract, leveraging cutting edge robotic and immunologic approaches to discover, characterise, and formulate novel small molecule adjuvants that may enhance vaccine responses of the young and the elderly. Dr Levy also leads US Friends of Children of Peace UK, an organisation that works to foster peaceful co-existence and friendship between Israeli and Palestinian children suffering from conflict. He lives in Cambridge, Massachusetts along with his wife Dr Sharon Levy and their three children. |
|
|---|---|---|
| 09:45 - 10:15 |
Nutritional factors modulating the neonatal immune response
The neonatal immune response may be modulated by the nutrition of a mother during gestation and by post-natal infant nutritional factors. In principle there are several pathways by which an expectant mother’s nutrition could modulate her baby’s immune response. This lecture will briefly outline: 1) existing evidence that nutritionally-mediated epigenetic changes occurring peri-conceptionally could preset immune responsiveness; 2) weak evidence that nutritional interventions could alter transplacental antibody transfer; and 3) evidence from prenatal supplementation trials with neonatal mortality as their endpoint. Post-natal nutrition could also modulate immune responses over and above the importance of early colostrum provision. This talk will focus on the two nutrients that have received greatest attention: vitamin A and iron. Meta-analysed evidence that very early administration of high-dose vitamin A could reduce early neonatal mortality was unclear with high heterogeneity between positive studies in Asia and null/negative studies in Africa. This prompted three major new trials that yielded similar results; some evidence of benefit in Asia, but evidence of harm in Africa. WHO currently does not recommend neonatal vitamin A. Iron is a major mediator of bacterial growth. Recent studies demonstrated that term neonates display a rapid hepcidin/IL6-mediated hypoferraemia and that post-natal serum is relatively bacteriostatic against common causes of neonatal septicaemia compared to cord serum. Further studies are underway to test whether premature and low-birthweight infants display the same protective response. Oral hepcidin agonists currently under development could potentially be deployed alongside antibiotics and hence augment the therapeutic arsenal in the face of antimicrobial resistance. 
Dr Sarah Prentice, London School of Hygiene & Tropical Medicine, UK

Dr Sarah Prentice, London School of Hygiene & Tropical Medicine, UKDr Sarah Prentice is a Wellcome Trust Clinical Fellow based at the London School of Hygiene and Tropical Medicine, and a paediatric trainee. Her research focuses on the potential immunological mechanisms underlying the non-specific effects of childhood immunisations. Most recently she has conducted a randomised controlled trial in Uganda, comparing the non-specific immune responses of infants receiving BCG at birth with those receiving it at 6 weeks of age. She is also involved in work in the Gambia investigating the impact of neonatal immunisations on the inflammatory-iron axis. This work seeks to identify whether enhancement of this axis may be useful in the prevention and treatment of neonatal infections. |
|
| 11:00 - 11:30 |
The role of breast milk on the infant microbiome and disease
The establishment of the infant microbiome has lifelong implications on health and immunity. The complex relationship between the microbial communities and infant immune development is only beginning to be realised. Multiple studies have shown the importance of breastfeeding in reducing chronic diseases such as atopy, diabetes, obesity and inflammatory bowel disease. This talk will review what is known about microbial communities in breast milk and microbial seeding of the infant gut through breastfeeding. 
Dr Pia S. Pannaraj, Keck School of Medicine, University of Southern California and Division of Infectious Diseases, Children’s Hospital Los Angeles, USA

Dr Pia S. Pannaraj, Keck School of Medicine, University of Southern California and Division of Infectious Diseases, Children’s Hospital Los Angeles, USAPia S. Pannaraj MD MPH is an Associate Professor of Clinical Pediatrics and Molecular Microbiology and Immunology at Keck School of Medicine, University of Southern California and Infectious Disease Specialist at Children’s Hospital Los Angeles. |
|
| 11:45 - 12:15 |
Manipulation of the neonatal microbiome – pitfalls and opportunities
Infections are the second most common cause of the estimated 4 million annual deaths in young children around the world. Compared to the achievements in combatting infections in infants and young children, the reduction in infectious morbidity and mortality in the newborn period has been inadequate. The majority of deaths due to infections occur in resource-poor settings. Novel simple, safe and affordable interventions to reduce the burden of infections in this population are therefore urgently needed and require careful and rigorous scientific assessment. Our understanding of the neonatal microbiome is evolving rapidly and emerging evidence highlights its relevance for short- and long-term health, including infectious diseases, cardiovascular and metabolic wellbeing as well as immune-mediated conditions such as asthma and allergies. Many well-intended routine perinatal interventions may have unexpected and lasting effects on the neonatal microbiome. This talk will review current knowledge relating to the ontogeny of the neonatal microbiome and its impact on health and disease. Further, it will explore the effects of current routine and potential future interventions on the neonatal microbiome, such as feeding practices, probiotic supplementation and neonatal skin care. 
Dr Tobias Strunk, King Edward Memorial Hospital for Women, Princess Margaret Hospital for Children and UWA Centre for Neonatal Research and Education, Australia

Dr Tobias Strunk, King Edward Memorial Hospital for Women, Princess Margaret Hospital for Children and UWA Centre for Neonatal Research and Education, AustraliaClinical Associate Professor Tobias Strunk is an early career clinical academic with a full-time appointment as consultant neonatologist in the NICU at King Edward Memorial and Princess Margaret Hospitals and the Centre for Neonatal Research and Education at the University of Western Australia. His research interests are the immunological determinants of new born susceptibility to invasive bacterial infection and novel prophylactic and therapeutic interventions to reduce disease burden. Dr Strunk’s research output is steadily growing, he has an excellent and growing track record for an early career researcher with 46 publications, >1000 citations and h-index of 18 (Google Scholar, 05/2016). Since the conferral of his PhD in 2012, he has secured $6.9M in independent research funding as Chief investigator for projects from various competitive funding sources. |
Chair

Professor Beate Kampmann, Imperial College London, UK and MRC Unit The Gambia

Professor Beate Kampmann, Imperial College London, UK and MRC Unit The Gambia
Professor Beate Kampmann holds a Chair in Paediatric Infection & Immunity at Imperial College, London and was appointed as the Scientific Director (Theme Leader) for Vaccinology research at the MRC Unit-The Gambia in July 2010. She leads a comprehensive childhood infection research program both in the UK and sub-saharan Africa, where she spends a third of her time. She has extensive practical and research experience in childhood infection for over 15 years and brings an established funding track record as PI and co-applicant from major international funders for the conduct of laboratory-based and programmatic research in TB and Vaccinology in both resource-poor and resource rich settings. At the MRC Unit in The Gambia, she directs all research activity in infant immunology, ranging from basic research of innate and acquired immune responses to infection and vaccination to clinical trials of novel vaccines and their adjuvants.
| 13:30 - 14:00 |
Current research in maternal immunisation
Immunisation of women during pregnancy is an accepted strategy to protect mothers and infants against infectious diseases during a period of high vulnerability. As a public health intervention, maternal immunisation has the potential to reduce the morbidity and mortality associated with pathogens that affect the mother, the newborn, or both. Maternal immunisation with tetanus, pertussis and influenza vaccines results in direct protection of the mother and the newborn infant. Group B streptococcus and Respiratory Syncytial Virus (RSV) are infections that could be prevented through immunisation of pregnant women with safe and effective vaccines that are currently under clinical investigation. This presentation will review the rationale, safety, effectiveness, acceptability and potential impact of the vaccination of women during pregnancy. Challenges associated with the development and implementation of clinical trials of vaccines administered during pregnancy will be discussed. 
Dr Flor Munoz-Rivas, Baylor College of Medicine, USA

Dr Flor Munoz-Rivas, Baylor College of Medicine, USAFlor M. Munoz MD, MSc. is Associate Professor of Pediatrics and Molecular Virology and Microbiology at Baylor College of Medicine (BCM) in Houston, Texas. Dr Munoz is a paediatric infectious diseases specialist interested in the epidemiology and prevention of infections in young infants through paediatric and maternal immunisation. She has over 18 years of experience in clinical research, conducting NIH and industry sponsored phase I to IV infant and maternal immunisation studies, and clinical trials of antiviral drugs for infants and children with respiratory infections. Dr Munoz is involved in CDC pandemic preparedness influenza projects that focus on surveillance, vaccine and antiviral effectiveness in hospitalised and ambulatory patients and pregnant women, and in the CDC NVSN ARI Surveillance Network. Dr Munoz is a member of the Committee of Infectious Diseases of the American Academy of Pediatrics, and COID liaison to the ACIP influenza working group. She is a member of special interest groups on maternal immunisation at NIH, CDC, WHO, NVAC, BM-Gates Foundation, and the Brighton Collaboration GAIA Project, which aims to achieve harmonisation of definitions for the assessment of safety of vaccines in pregnancy. She is IRB Chair at BCM, Director of the Solid Organ Transplant Infectious Diseases Program and Infectious Diseases Consultant at Texas Children's Hospital in Houston, TX. |
|
|---|---|---|
| 14:15 - 14:45 |
Current research in neonatal immunisation
The current vaccine schedule has successfully reduced the incidence of serious infectious diseases in young children and the majority of deaths in children less than five years now occur in the neonatal period, with neonatal infections accounting for up to a third of deaths in newborns. A number of challenges exist to neonatal vaccination including safety concerns (both immunological and clinical), demonstration of vaccine efficacy and public acceptance. Recent advances in our understanding of neonatal immunology have led to a renewed interest in neonatal immunisation. Currently hepatitis B, polio and the BCG vaccine are given at birth. Hepatitis B vaccine is effective at reducing mother to child transmission of infection, but long-term protection remains under investigation. The BCG vaccine has up to 80% efficacy at protecting newborns and infants from disseminated TB disease. Recent studies of acellular pertussis and pneumococcal vaccine given at birth have proven they are well tolerated and immunogenic. Ongoing research to understand how neonatal vaccine responses are elicited, and to identify optimal adjuvants and formulations is required to reduce the disease burden in this group. 
Dr Elizabeth Whittaker, Imperial College London, UK

Dr Elizabeth Whittaker, Imperial College London, UKDoctor Elizabeth Whittaker is an Academic Clinical Lecturer in Paediatric Infectious Diseases and Immunology at Imperial College London. Her main research interests are age-related immune responses to infectious diseases, in particular infants under a year of age. She completed her undergraduate training in medicine at Trinity College, Dublin, Ireland, including an HRB (Health Research Board) funded BSc in Immunology. Following this she trained as a paediatrician in London and was successfully awarded an Academic Clinical Fellowship in Paediatric Infectious diseases. She completed her Wellcome Trust funded PhD ‘Age-related immune responses to Mycobacteria’ in the laboratories of Professor Beate Kampmann at Imperial College and Professors Mark Nicol and Heather Zar at the University of Cape Town. She divides her time between clinical work, research and teaching, and practising as a paediatric Consultant at St. Marys Hospital, London. |
Chair

Dr Chrissie Jones, St George's, University of London, UK

Dr Chrissie Jones, St George's, University of London, UK
Dr Chrissie Jones is an Associate Professor in Paediatric Infectious Diseases at the University of Southampton. Her research interests include interventions in pregnancy to prevent infection in early life. She has particular expertise in the field of maternal vaccination and leads pertussis and RSV clinical trials in pregnancy. She serves on the executive committee of GAIA (http://gaia-consortium.net), a large international consortium. As part of this initiative, Dr Jones has authored international guidelines to provide a standard for data collection in clinical trials of vaccines in pregnancy, which are recommended by the WHO.
Dr Jones is the chief investigator of RACE-FIT, a NIHR-funded feasibility study to assess an educational intervention to reduce the risk of CMV acquisition in pregnancy.
With postgraduate training in medical education, Dr Jones is involved with multiple initiatives to train and equip others in paediatric infectious diseases.

Dr Elizabeth Whittaker, Imperial College London, UK

Dr Elizabeth Whittaker, Imperial College London, UK
Doctor Elizabeth Whittaker is an Academic Clinical Lecturer in Paediatric Infectious Diseases and Immunology at Imperial College London. Her main research interests are age-related immune responses to infectious diseases, in particular infants under a year of age. She completed her undergraduate training in medicine at Trinity College, Dublin, Ireland, including an HRB (Health Research Board) funded BSc in Immunology. Following this she trained as a paediatrician in London and was successfully awarded an Academic Clinical Fellowship in Paediatric Infectious diseases. She completed her Wellcome Trust funded PhD ‘Age-related immune responses to Mycobacteria’ in the laboratories of Professor Beate Kampmann at Imperial College and Professors Mark Nicol and Heather Zar at the University of Cape Town. She divides her time between clinical work, research and teaching, and practising as a paediatric Consultant at St. Marys Hospital, London.

Dr Kirsty Le Doare, Imperial College London, UK

Dr Kirsty Le Doare, Imperial College London, UK
Dr Kirsty Le Doare is a consultant in paediatric infection and immunology at Evelina London Children’s Hospital and a Wellcome Trust Fellow at Imperial College London. Her main research interests are age-related immune responses to infectious diseases, in particular to Group B-streptococcus in neonates.
Kirsty is a late starter to medicine, having spent ten years working as an economist for NGOs such as Oxfam, following completion of a joint BA (Hons.) degree/Diplom-Betriebswirtin in European Economic Studies as part of an ERASMUS link between universities in the UK, Germany, Spain and France. Her experience in developing countries led her to enter post-graduate medical training at St. George's University of London. She was successfully awarded an Academic Specialty Training in International Child Health in 2008. She was awarded a prestigious sub-specialty training post in Paediatric Immunology and Infectious Diseases in 2012, the Oxford Masters in Paediatric Infectious Diseases in 2014 and now works as a clinical academic between the Evelina Children’s Hospital, Imperial College London and MRC The Gambia.
Kirsty is currently leading an international collaboration to standardise assays to measure antibody against Group B Streptococcus with the aim of facilitating the development of an immune correlate of protection against GBS colonisation and disease.
Kirsty is a member of the Royal College of Paediatrics and Child Health (MRCPCH), Academic Paediatrics Association (APA), British Paediatric Allergy Infection and Immunity Group (BPAIIG), Children's HIV Association (CHIVA) and International Child Health Group.
| 15:30 - 16:15 | Breakout session: Future strategies for maternal immunisation |
|---|---|
| 15:30 - 16:15 | Breakout session: Future strategies for neonatal immunisation |
| 15:30 - 16:15 | Breakout session: Other immunomodulatory strategies |
| 16:15 - 17:00 | Summary of discussions and closing remarks |
