Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Integrated control of cerebral blood flow
Theo Murphy international scientific meeting organised by Professor Stephen Payne, Dr Clare Howarth, Professor Daniel Bulte and Professor Shieak Tzeng
The brain regulates cerebral blood flow very tightly to provide a sufficient and continuous supply of oxygen and glucose. It thus has to respond to many different challenges, which have traditionally been considered largely separately. In this meeting we aimed to move towards an integrated approach to understanding cerebral blood flow control and to explore its important clinical implications.
The schedule of talks and speaker abstracts and biographies are below. Recorded audio of the presentations will be available on this page after the meeting has taken place.
This was a residential conference, which allows for increased discussion and networking.
Attending this event
This event has taken place.
Enquiries: contact the Scientific Programmes team
Organisers
Schedule
Chair

Professor Daniel Bulte, University of Oxford, UK

Professor Daniel Bulte, University of Oxford, UK
Professor Daniel Bulte is an MRI physicist and an Associate Professor in Engineering Science at the University of Oxford. He is based at the Institute of Biomedical Engineering (IBME) and previously worked at the Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (FMRIB) for over 10 years, and the University of Toronto before that. He obtained a PhD in Electrical Engineering and a BSc in Physics from the University of Tasmania in Australia. He is a Senior Fellow of the Higher Education Academy, and has a Postgraduate Diploma in Learning and Teaching in Higher Education from Oxford University. He is passionate about teaching and outreach and has won numerous awards for his teaching.
| 09:00 - 09:05 | Welcome session | |
|---|---|---|
| 09:05 - 09:30 |
Flow/Pressure Sensing by Ion Channels and the Setting of Cerebral Arterial Tone Development
Brain perfusion is controlled by an arterial network, responsive to stimuli that grades membrane potential (VM) and Ca2+ influx. Arterial VM is set by an interplay among ion channels, each uniquely expressed in smooth muscle or endothelium. Inward rectifying K+ (KIR) channels break from convention in the cerebral circulation, an observation consistent with KIR being more than resting current. Recent work has noted that KIR might be sensitive to haemodynamics forces due to their interaction with membrane lipids. In this regard, Professor Welsh and his team examined the regulation of cerebral arterial KIR channels by membrane lipids (PIP2 and cholesterol) and whether these signalling molecules enable channel mechanosensitivity. Initial experiments revealed a Ba2+-sensitive KIR current in native cerebral arterial smooth muscle and endothelial cells comprised of KIR2.1 and KIR2.2 subunits. Patch clamp observations next noted that endothelial KIR was regulated by PIP2 whereas membrane cholesterol was the main modulator of smooth muscle KIR. Further work revealed that smooth muscle KIR displays pressure-sensitivity when bound to membrane cholesterol whereas endothelial KIR shows flow-sensitivity when coupled to PIP2. Using computer models, the team integrated these observations to reveal how each cellular KIR pool controls arterial VM and tone. The researchers propose that specific membrane lipid-KIR interactions allow each cellular channel pool to sense haemodynamic stimuli, thus set the foundation of tone development and perfusion control in the cerebral circulation. 
Professor Donald Welsh, University of Western Ontario, Canada

Professor Donald Welsh, University of Western Ontario, CanadaDonald G Welsh is a Scientist at the Robarts Research Institute, Professor in the Department of Physiology & Pharmacology (Schulich School of Medicine & Dentistry) at Western University and the Rorabeck Chair in Neuroscience and Vascular Biology. His research focuses on ion channels and cellular mechanisms by which these membrane proteins regulate arterial tone development. His most significant contributions include: 1) quantification of electrical communication in resistance arteries, work that has fostered a deeper understanding of excitation-contraction coupling in vascular smooth muscle; 2) characterization and function of Ttype Ca2+ channels, elusive membrane proteins which appear to play a key role in gating of large co ductance Ca2+-activated K+ channels; and 3) defining the basis of myogenic tone, work that entailed the development of new biochemical, Ca2+imaging and myography approaches. The latter is of particular importance to the blood pressure regulation and the control of blood flow delivery to the brain. |
|
| 09:30 - 09:45 | Discussion | |
| 09:45 - 10:15 |
Models of cerebral autoregulation
There is a very wide literature covering models of cerebral autoregulation. The early work of Ursino and colleagues has been very widely adopted and adapted, although the feedback mechanisms remain somewhat imprecisely defined and the parameter values recovered experimentally have proved difficult to interpret. This has also made it challenging to link models of cerebral autoregulation with models in other contexts. More recent models have attempted to understand both the interaction between the responses to different stimuli and to dig deeper into the physiological mechanisms that govern autoregulation. In this talk, Professor Payne will give an overview of existing models of cerebral autoregulation, starting with high level models that tend to be based on a lumped compartment approach, before turning to consider the response of individual blood vessels in more detail. He will then explore how these physiological models might be combined in the future to develop models across multiple length scales that might be applicable to experimental data and help to interrogate the response in more detail. Such models also open up the possibility of linking with models of different responses, such as reactivity and neurovascular coupling, and thus potentially providing a more coordinated approach that can be used within a clinical setting to interrogate the cerebral vasculature and its regulation of blood flow in response to multiple stimuli. 
Professor Stephen Payne, University of Oxford, UK

Professor Stephen Payne, University of Oxford, UKProfessor Stephen Payne is an Associate Professor in in Biomedical Engineering at the Institute of Biomedical Engineering, part of the Department of Engineering Science (and winner of a Queen’s Anniversary Prize for Higher and Further Education in 2015) at the University of Oxford. His work lies primarily in mathematical modelling and signal processing related to cerebral blood flow and metabolism with the main focus on cerebral autoregulation. He has raised funding of over £1.2M in grants as a PI and been a Co-Investigator on three other grants (with a share of £1.3M), with funding coming from EPSRC, BBSRC, Wellcome Trust and the European Commission. His publications include three books (including Cerebral Autoregulation in 2016 and Cerebral Blood Flow and Metabolism in 2017), and 90 papers in international journals (h-index of 21 with over 1300 citations). He has supervised 23 DPhil students to successful completion. He is currently the Chair of CARNet and the Chair of the Organising Committee for both the 8th International Conference on Cerebral Autoregulation (June 2018) and the Royal Society meeting on Integrated Control of Cerebral Blood Flow (December 2018). |
|
| 10:15 - 10:30 | Discussion | |
| 10:30 - 11:00 | Coffee | |
| 11:00 - 11:30 |
Experimental Approaches for Assessment of Cerebral Autoregulation in Humans
Classically, cerebral autoregulation has been defined as the maintenance of relatively stable cerebral blood flow across a finite range of arterial pressures, facilitated by active adjustments in cerebral vascular resistance. Initial assessment of cerebral autoregulation in humans incorporated static measurements of arterial pressure and cerebral blood flow using invasive techniques (inert gas inhalation, and indwelling venous and arterial catheters). With the development of advanced monitoring technologies that facilitate non-invasive capture of continuous arterial pressure and cerebral blood flow (or velocity), the dynamic relationship between cerebral blood flow and arterial pressure has been extensively explored. Non-invasive examination of cerebral tissue oxygenation as a primary end-point of cerebral autoregulation is also gaining popularity both in the experimental and clinical settings. These assessments have been made using recordings of spontaneous variations in arterial pressure and cerebral blood flow (and/or oxygenation), as well as forced or induced fluctuations. Common methods for inducing fluctuations in arterial pressure include the squat-to-stand test, lower body negative pressure, and thigh cuff inflation/deflation. In this presentation, the strengths and limitations of these methodological approaches for assessment of static and dynamic cerebral autoregulation will be presented and discussed, including application to the clinical setting. 
Associate Professor, Caroline Rickards, University of North Texas Health Science Center, USA

Associate Professor, Caroline Rickards, University of North Texas Health Science Center, USADr Caroline Rickards is an Associate Professor in the Department of Physiology & Anatomy at the University of North Texas Health Science Center in Fort Worth, Texas, USA. She is Director of the Cerebral & Cardiovascular Physiology Laboratory where her research focuses on the development of novel therapies to improve vital organ perfusion under stress (including hemorrhage, cardiac arrest, and stroke). She has received funding for this research from the US Department of Defense, the American Heart Association, private foundations, and industry contracts. Dr Rickards is also an active member within her professional societies, including service on a number of committees within the American Physiological Society, Secretary of the Cerebral Autoregulation Research Network (CARNet), and editorial board membership for the Journal of Physiology and the American Journal of Physiology – Regulatory, Integrative and Comparative Physiology. |
|
| 11:30 - 11:45 | Discussion | |
| 11:45 - 12:15 |
Cerebral dysautoregulation in acute stroke – implications for the management of haemodynamic perturbations
Stroke is a leading cause of mortality and long-term adult disability, and of increasing importance with demographic population changes. Physiological perturbations, particularly with respect to systemic (eg blood pressure) and cerebral haemodynamics (eg cerebral blood flow), are common following both acute ischaemic and haemorrhagic stroke. Importantly, mechanisms that control cerebral blood flow, including cerebral autoregulation, are impaired in the acute and sub-acute period. It is vital to understand these to inform the acute management of these physiological perturbations, particularly in the context of acute stroke treatment developments, including pharmacological and mechanical reperfusion therapies. Therefore, the talk will consider: 1) the evidence for cerebral dysautoregulation in acute ischaemic and haemorrhagic stroke; 2) recent developments in pharmacological and mechanical reperfusion therapies; 3) current guidelines for blood pressure management in acute ischaemic and haemorrhagic stroke; and 4) implications for future cerebral autoregulation research. 
Professor Thompson Robinson, University of Leicester, UK

Professor Thompson Robinson, University of Leicester, UKProfessor Tom Robinson undertook his medical training in Nottingham, Newcastle-Upon-Tyne and Leicester, and is currently Head of the Department of Cardiovascular Sciences and Professor of Stroke Medicine at the University of Leicester, and also an Honorary Consultant Physician in Stroke Medicine for University Hospitals of Leicester NHS Trust. He was appointed an NIHR Senior Investigator in April 2016. His other responsibilities include: Chair of the Membership Committee of the European Stroke Organisation, President of the British Association of Stroke Physicians, and National Specialty Lead for Stroke for the NIHR Clinical Research Network. His research interests include clinical trials in acute stroke, particularly blood pressure and thrombolysis management, and studies of cardiovascular and cerebrovascular regulatory mechanisms. His research is currently funded by the British Heart Foundation, the Stroke Association, the Engineering and Physical Sciences Research Council, and the National Institute of Health Research. |
|
| 12:15 - 12:30 | Discussion |
Chair

Professor Stephen Payne, University of Oxford, UK

Professor Stephen Payne, University of Oxford, UK
Professor Stephen Payne is an Associate Professor in in Biomedical Engineering at the Institute of Biomedical Engineering, part of the Department of Engineering Science (and winner of a Queen’s Anniversary Prize for Higher and Further Education in 2015) at the University of Oxford. His work lies primarily in mathematical modelling and signal processing related to cerebral blood flow and metabolism with the main focus on cerebral autoregulation. He has raised funding of over £1.2M in grants as a PI and been a Co-Investigator on three other grants (with a share of £1.3M), with funding coming from EPSRC, BBSRC, Wellcome Trust and the European Commission. His publications include three books (including Cerebral Autoregulation in 2016 and Cerebral Blood Flow and Metabolism in 2017), and 90 papers in international journals (h-index of 21 with over 1300 citations). He has supervised 23 DPhil students to successful completion. He is currently the Chair of CARNet and the Chair of the Organising Committee for both the 8th International Conference on Cerebral Autoregulation (June 2018) and the Royal Society meeting on Integrated Control of Cerebral Blood Flow (December 2018).
| 13:30 - 14:00 |
Effects of Aerobic Exercise on Cerebrovascular Health in Older Adults: Insights from the Brain in Motion Study

Professor Marc Poulin, University of Calgary, Canada

Professor Marc Poulin, University of Calgary, CanadaMarc Poulin is Professor of Physiology in the Cumming School of Medicine (Departments of Physiology & Pharmacology, and Clinical Neurosciences) and the Faculty of Kinesiology at the University of Calgary. He is a member of the Hotchkiss Brain Institute, the Libin Cardiovascular Institute of Alberta, and the O’Brien Institute of Public Health at the University of Calgary. He also holds the Brenda Strafford Foundation Chair in Alzheimer Research. He obtained a Bachelor of Physical and Health Education (Honors) from Laurentian University (Sudbury, Ontario; 1986), an MA and PhD in Exercise Physiology from the University of Western Ontario (London, Canada; 1988 and 1993) and a DPhil in Respiratory and Cerebrovascular Human Physiology from the University of Oxford (New College; Oxford, UK; 1999). His research focuses on the mechanisms of cerebrovascular regulation and perturbations in blood gases in health and disease. His two primary research areas include i) healthy brain aging and dementia (focusing on the impact of exercise on cerebral blood flow and cognitive function), and ii) the effects of intermittent hypoxia in health (using experimental human models), in workers who work at high altitude, and in the pathogenesis of obstructive sleep apnea. He holds grant funding from the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada, and the Heart and Stroke Foundation of Canada. |
|
|---|---|---|
| 14:00 - 14:15 | Discussion | |
| 14:15 - 14:45 |
Cerebrovascular reactivity: biomarker or target?
Impairments in cerebrovascular reactivity have been recognised as a comorbidity in a broad range of neurological conditions including Alzheimer’s disease, multiple sclerosis, MCI, Parkinson’s disease, stroke, and even depression. There has been a recent move to consider that CVR could be useful as a biomarker for dementia, but its near ubiquitous presence in neurological diseases means it has often been considered as lacking the required specificity to be a biomarker. Professor Bulte poses the question ‘Is impaired CVR in fact the root cause of damage that results in these conditions?’ CVR regulates the availability of oxygen to the brain on a minute by minute basis. Lack of adequate oxygen is clearly catastrophic for tissues in the brain. Instead of being a potential biomarker for diagnosing a particular condition, what if impaired CVR should be the treatment target? The Bulte group can measure regional CVR and have identified that groups with an elevated risk of a number of diseases all have impaired CVR decades before it would be expected to observe any other diagnosable symptoms. The breakthrough in treating many of these conditions may be preventing them by addressing the CVR impairments early in life rather than waiting for other symptoms to arise and getting lost in a forest of biomarkers. 
Professor Daniel Bulte, University of Oxford, UK

Professor Daniel Bulte, University of Oxford, UKProfessor Daniel Bulte is an MRI physicist and an Associate Professor in Engineering Science at the University of Oxford. He is based at the Institute of Biomedical Engineering (IBME) and previously worked at the Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (FMRIB) for over 10 years, and the University of Toronto before that. He obtained a PhD in Electrical Engineering and a BSc in Physics from the University of Tasmania in Australia. He is a Senior Fellow of the Higher Education Academy, and has a Postgraduate Diploma in Learning and Teaching in Higher Education from Oxford University. He is passionate about teaching and outreach and has won numerous awards for his teaching. |
|
| 14:45 - 15:00 | Discussion | |
| 15:00 - 15:30 | Tea | |
| 15:30 - 16:00 |
MRI of cerebrovascular reactivity: applications and caveats
Cerebrovascular reactivity (CVR) is measured as the quantitative haemodynamic response to a vasodilatory challenge. This is typically done as the response to a hypercapnic challenge and measured either using trans-cranial Doppler (TCD) or magnetic resonance imaging (MRI). MRI allows local measurement both in terms of the blood oxygen level-dependent (BOLD) signal and arterial spin labelling (ASL) perfusion measures. A higher CVR is typically interpreted as a sign of greater cerebral vascular health. Professor Gauthier and her team’s work in older adults show that overall trends across the lifespan support this interpretation, but results obtained in relation to cardiorespiratory fitness indicate a more complex relationship between fitness and haemodynamics. Results suggest that in healthy older adults, CVR is in fact negatively correlated with fitness over much of grey matter. Within the regions showing this negative relationship, the group further identified a negative relationship between VO2 max and both perfusion and perfusion-based CVR measured using ASL. These results also indicate that there are caveats to using BOLD CVR as a quantitative measure of cerebrovascular health. Here these results, their impact on the group’s interpretation of different types of CVR measurements and possible interpretations and future avenues of research will be discussed. 
Professor Claudine Gauthier, Concordia University/Montreal Heart Institute, Canada

Professor Claudine Gauthier, Concordia University/Montreal Heart Institute, CanadaClaudine Gauthier is an Assistant Professor in the Department of Physics at Concordia University and a researcher at the Montreal Heart Institute. Her research explores the quantification of physiological changes in the brain using MRI during aging, vascular diseases, and preventative interventions such as exercise and cognitive training. Dr Gauthier did her PhD in Neuroscience at Université de Montréal with Dr Richard Hoge on the development of calibrated fMRI methods for quantification of brain metabolism, and the study of aging-related changes in vascular and metabolic health. Her post-doctoral work at the Max Planck Institute for Human Cognitive and Brain Sciences in Leipzig with Dr Robert Turner and Dr Arno Villringer explored the use of ultra-high field MRI for enhanced metabolic quantification and quantitative multi-modal MRI of learning-induced plasticity. Dr Gauthier is the co-founder of the Imaging Cerebral Physiology network and is currently the recipient of the Heart and Stroke Foundation of Canada New Investigator Award and the Henry JM Barnett Scholarship for her work on stroke. |
|
| 16:00 - 16:15 | Discussion | |
| 16:15 - 16:45 |
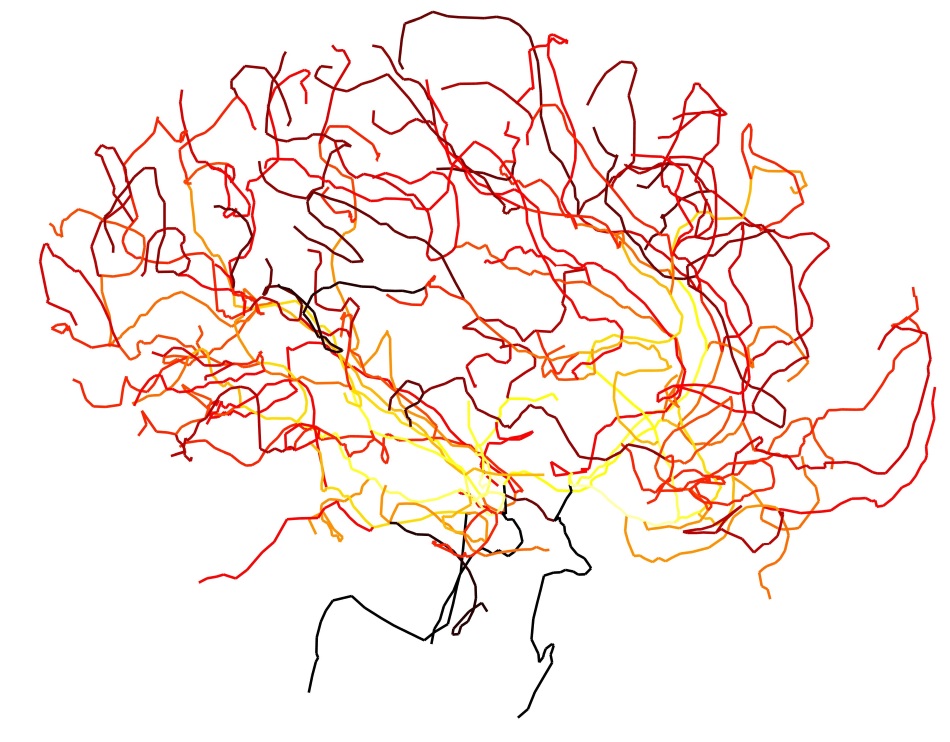
Mapping Cerebral Blood Flow Regulation in Aging and Dementia
The brain is highly metabolic demanding 20% of the cardiac output with healthy vascular function critical for delivering metabolites and removing waste. Both acute and chronic vascular dysfunction lead to tissue injury differing only in the pace of neuronal loss with acute ischaemic stroke and vascular dementia (VaD) representing both ends of the spectrum. Importantly, recent research evidence has inferred that Alzheimer’s Dementia (AD) may be initiated by vascular dysfunction. Since greater than 90% of dementia is secondary to AD or VaD, understanding the relationship between vascular function and dementia is critical. Recent statistics show that in the last five years of life, the cost of dementia is virtually equal to that of heart disease and cancer combined. However, measurement of cerebral blood flow (CBF) has not proven effective for assessing dementia due to: 1) autoregulatory compensation with maintenance of normal CBF in the setting of vasculopathies; 2) wide variations in normal resting CBF; and 3) difficulties in measuring CBF accurately. Therefore, understanding the impact of deficiencies in the flow control system must do more than measure resting CBF alone. It must investigate the capacity and integrity of the control mechanism itself. The purpose of this presentation therefore is to explore the relationship between CBF regulation, ageing, and dementia. The method used applied utilises quantitative vasodilatory stimuli during MRI to generate maps of the speed and magnitude of blood flow responses over the entire brain. Concepts and data will be presented to support the potential efficacy of this approach. 
Professor David Mikulis, University of Toronto, Canada

Professor David Mikulis, University of Toronto, CanadaDavid J Mikulisis is Full Professor and Director of the Functional Brain Imaging Lab in the Dept. of Medical Imaging at the University of Toronto and the University Health Network in Toronto. He is also a Senior Scientist at the Toronto Western Research Institute and Co-Chair of the Vessel Wall Imaging International Study Group of the American Society of Neuroradiology. The primary emphasis of his work has been translational research focusing on the application of novel imaging methods to the clinical environment. He established one of the first fMRI labs in Canada in 1993 and is currently involved in developing advanced neurovascular imaging methods with major program arms including: 1) quantitative measurement and clinical application of cerebrovascular reactivity (CVR) metrics via precision control of blood oxygen and carbon dioxide, 2) high resolution and functional imaging of intra and extra-cranial blood vessel walls. Work in these areas has led to improved understanding of neurovascular uncoupling that may explain the origin of chronic ischemic white matter injury a major contributor to vascular dementia, and 3) imaging the glymphatic system. |
|
| 16:45 - 17:00 | Discussion |
Chair

Dr Clare Howarth, University of Sheffield, UK

Dr Clare Howarth, University of Sheffield, UK
Clare undertook a PhD at University College London on the Wellcome Trust 4 year PhD program in Neuroscience. Working with David Attwell, she discovered a new mechanism for the control of brain blood flow at the capillary level and produced the first energy budget for the cerebellum. Following her PhD, she was awarded a Sir Henry Wellcome Postdoctoral Fellowship which enabled her to work with Brian MacVicar (University of British Columbia), applying two-photon microscopy to brain slices, and with Nicola Sibson (Oxford), using in vivo MRI and optical imaging techniques to elucidate the role of astrocytes in regulating cerebral blood flow responses to hypercapnia. In October 2013 she moved to the University of Sheffield, where she was recently awarded a Sir Henry Dale Fellowship by the Wellcome Trust and Royal Society to investigate the role of astrocytes in neurovascular coupling in health and aging.
| 09:00 - 09:30 |
Balancing the brain’s energy supply: neurovascular coupling in the cortex and hippocampus
Neurovascular coupling has been predominantly studied in primary sensory cortices, where neuronal activation leads to increased cerebral blood flow and a large influx of oxygenated blood. However, neural activity may be less well-coupled to increased blood flow in other brain areas. For example, local field potentials are highly correlated with fMRI/BOLD signals in sensory cortex, but not in the hippocampus (Ekstrom, 2010), suggesting neurovascular coupling may differ between sensory cortex and hippocampus. To investigate this directly, Dr Hall and her team used 2-photon imaging to record fluctuations in neuronal activity and microvascular diameter in primary visual cortex (V1) and the hippocampus of awake, behaving mice, as well as combined laser doppler flowmetry and haemoglobin spectroscopy to record baseline and stimulus-induced alterations in macroscopic haemodynamics. Compared to V1, the hippocampus had lower resting blood flow and blood oxygen saturation, despite similar rates of oxygen consumption. Furthermore, individual blood vessels dilated significantly less frequently and to a smaller extent in the hippocampus compared to V1, despite equivalent-sized calcium responses. Finally, increases in regional oxygen consumption led to smaller macroscopic increases in blood flow in the hippocampus compared to V1. These data suggest that not only is the hippocampus under-supplied with oxygen compared to primary sensory cortex at rest, but it is also less able to increase local blood flow in response to increased neuronal activity. These deficits in neurovascular coupling could contribute to the vulnerability of the hippocampus to hypoxia by reducing the ability of hippocampal neurons to match energy supply with demand. 
Dr Kira Shaw, University of Sussex

Dr Kira Shaw, University of SussexKira Shaw is interested in the supply and regulation of energy in the brain (neurovascular coupling) across different brain states and regions. During her PhD (with Jason Berwick, University of Sheffield), she studied how neurovascular coupling relationships are altered by arousal levels (in awake mice, i.e. aroused/locomotion and quiescent/rest) or anaesthesia. In her current position as a post-doctoral researcher (with Catherine Hall, University of Sussex) she compares how the brain’s control of blood flow may differ between cortex and hippocampus, and how this might impact upon brain function. |
|
|---|---|---|
| 09:30 - 09:45 | Discussion | |
| 09:45 - 10:15 |
Building a mathematical model of brain energy metabolism
The brain consumes an inordinate amount of energy with respect to its weight. Understanding brain energy metabolism is crucial as numerous studies point to a metabolic component in various neurodegenerative disorders and because energetic considerations might have played an important role during evolution, constraining behaviour and providing a powerful explanation of certain cellular features as trade-offs between performance in information processing and energy savings. Professor Jolivet will briefly discuss these points before describing how to design models of brain energy metabolism and neurovascular coupling, the importance of calibration due to the multicellular complexity of the brain and algorithmic tools to analyse the behaviour of such models. The brain consumes an inordinate amount of energy with respect to its weight. Understanding brain energy metabolism is crucial as numerous studies point to a metabolic component in various neurodegenerative disorders and because energetic considerations might have played an important role during evolution, constraining behaviour and providing a powerful explanation of certain cellular features as trade-offs between performance in information processing and energy savings. Professor Jolivet will briefly discuss these points before describing how to design models of brain energy metabolism and neurovascular coupling, the importance of calibration due to the multicellular complexity of the brain and algorithmic tools to analyse the behaviour of such models. 
Professor Renaud Jolivet, University of Geneva and CERN, Switzerland

Professor Renaud Jolivet, University of Geneva and CERN, SwitzerlandRenaud Jolivet studied theoretical biophysics at the University of Lausanne (1996-2001) before doing a PhD in computational neuroscience at École polytechnique fédérale de Lausanne in Lausanne, Switzerland (2001-2005). After his doctoral studies, he was a postdoc in Lausanne (2006-2007) and a fellow in Tokyo, Zürich and London (2007-2015). Since 2016, he is Joint Titular Professor in Medical Physics at CERN and at the University of Geneva, Switzerland. His main interest lies in the organization of brain energy metabolism and in the relation between energy consumption and information processing in neural networks, which his team studies in both experiments and computational models. He also holds a particular interest in the non-neuronal cells of the brain. |
|
| 10:15 - 10:30 | Discussion | |
| 10:30 - 11:00 | Coffee | |
| 11:00 - 11:30 |
Neuronal activity and neuroenergetics with and without CBF
Neurons in the brain rely on blood vessels for supply of oxygen and glucose. An increase in neuronal activity normally leads to vasodilation increasing cerebral blood flow (CBF), so that supply meets demand. Dilation is driven by multiple mechanisms emphasising its importance for healthy brain function. Vasoactive messengers are released by different types of neurons and possibly glia. In addition, blood vessels are endowed with an array of ion channels that propagate the signal along their walls ensuring “upstream” dilation magnifying the CBF response. But what happens to the oxygen and glucose? According to standard textbooks, brain’s energy is produced mostly by the oxidation of glucose to carbon dioxide and water. This notion is based on observations that cortical neuronal activity is lost within ~15 seconds of CBF interruption. A paradox that challenges this paradigm comes from Positron Emission Tomography studies, where glucose consumption was shown to exceed the oxygen consumption predicted by the stoichiometry of complete aerobic oxidation. Most of the brain’s grey matter energy is used to restore neuronal membrane potential that involves moving ions across against their concentration gradients. Therefore, Dr Devor and her team asked whether the ability of neurons to repolarise was lost within seconds of CBF interruption. Cortical neurons in the mouse brain, when repeatedly depolarised via light-controlled ion channels, continued to restore their membrane potential for over 20 minutes after a cardiac arrest. This observation suggests that neurons can utilise oxygen-independent mechanisms such as glycolysis, possibly not only upon asphyxia but also under normal physiological conditions. 
Dr Anna Devor, University of California, San Diego, USA

Dr Anna Devor, University of California, San Diego, USAAnna Devor holds two academic appointments as Associate Adjunct Professor in Neurosciences and Radiology at University of California San Diego (UCSD) and Instructor in Radiology at Massachusetts General Hospital (MGH, Harvard Medical School). Dr Devor has a broad base of knowledge in cellular and systems-level neuroscience. Her secondary expertise is development and refinement of microscopic optical technology for imaging of brain activity in live animals (in vivo). Dr Devor received her initial research training at the interface between experimental and computational neuroscience at Hebrew University of Jerusalem, Israel. Her PhD thesis focused on biophysical mechanisms of the membrane potential oscillations in a network of electrically coupled neurons. After completing her PhD in 2001, she went on to specialise in optical and MR-based imaging technology at Martinos Center for Biomedical Imaging at MGH before taking up an independent position as Instructor in Radiology at the same institution in 2004. In 2005, she accepted a second academic appointment at UCSD. The core of Dr Devor’s research program is focused on dissecting neuronal, glial and vascular mechanisms that underlie signals obtained with noninvasive brain imaging modalities such as fMRI. She has published extensively on imaging and recording of brain activity using 2-photon microscopy, voltage- and calcium-sensitive sensors, O2-sensitive phosphorescent probes, intrinsic optical contrasts and extracellular electrophysiological recordings. These microscopic measurements are integrated in a computational framework that allows prediction of macroscopic fMRI responses. Dr Devor also applies novel imaging technologies for in vivo investigation of mouse models of neurological disease and human stem cell-derived neurons transplanted in the mouse brain. |
|
| 11:30 - 11:45 | Discussion | |
| 11:45 - 12:15 |
The neurovascular unit in health and disease: lessons from animal models
The concept of neurovascular unit (NVU) emerged from the first Stroke Progress Review Group meeting of the National Institutes of Health in the year 2000, to highlight the close developmental, structural and functional interactions between neurons, glia and the cerebral vasculature.The NVU concept emphasised the symbiotic relationship between brain cells and cerebral blood vessels in health and disease. Over the past 18 years, the NVU construct has evolved considerably. In addition to astrocytes, neurons, smooth muscle cells, and endothelium, new cell types have emerged as critical components of the NVU, such as pericytes and perivascular macrophages, etc. The extracellular matrix, matrix proteases and basement membranes (matrisome) constitute an integral part of the NVU. The NVU has also emerged as a guardian of innate and adaptive immune homeostasis and as a key regulator of the trafficking of immune cells in and out of the brain. New trophic interactions have been discovered between vascular cells and brain cells (neurons, astrocytes and oligodendrocytes), which are essential for brain survival and repair. Furthermore, the NVU is involved in the clearance of unwanted molecules from the brain and in proteostasis through the blood–brain barrier (transvascular pathway) or the perivascular space (peri- and para-vascular pathways). These critical functions of the NVU are impaired by vascular risk factors, eg, hypertension, by ageing and by pathological changes associated with Alzheimer’s disease. Consequently the NVU has taken centerstage in a wide variety of brain diseases, but particularly in conditions associated with cognitive impairment. This presentation will provide a brief overview of the structure and function of the NVU and of its critical role in brain function and cognitive health. 
Professor Costantino Iadecola, Weill Cornell Medicine, USA

Professor Costantino Iadecola, Weill Cornell Medicine, USAProfessor Costantino Iadecola is the Director and Chair of the Brain and Mind Research Institute at Weill Cornell Medicine. He has published over 300 journal articles and plays a leadership role in national and international networks for stroke and dementia research. Dr Iadecola is a recipient of two Javits Awards (2009 and 2015) from the National Institutes of Health, the Willis Award from the American Heart Association (AHA), and of the Zenith Fellow Award from the Alzheimer’s Association. In 2015 he received the Excellence Award for Hypertension Research (Novartis-AHA), in recognition of his seminal work on Alzheimer’s disease pathology and hypertension. He is on the editorial boards of several journals and has been active in various editorial capacities for Stroke, Hypertension, Circulation, the Proceedings of the National Academy of Sciences, and the Journal of Neuroscience. In 2015 he was elected to the Association of American Physicians. Dr Iadecola is currently the Principal Investigator of several NIH grants and of grants from the Leon Levy Foundation and the Leducq Foundation. |
|
| 12:15 - 12:30 | Discussion |
| 13:30 - 14:00 |
Role of cerebral conduit arteries in cerebral blood flow adjustments
This presentation will summarise Professor Shoemaker and his team’s efforts to study the dynamic properties of basal conduit artery dilation and constriction in health and disease with additional preliminary studies on endothelial contributions to their cross-sectional area. Understanding cerebral blood flow (CBF) control has benefited dramatically from the non-invasive method of transcranial Doppler ultrasound which offers high temporal resolution, providing information regarding cerebral perfusion pulsatility to rapid postural adjustments in overall flow. However, these data are obtained from the basal conduit arteries under the major assumption that these vessels express very little reactivity to dilatory or constrictor stimuli so that their cross-sectional area remains constant. In this view, changes in flow velocity relate well to changes in total CBF. However, new applications with ultrasound imaging as well as high field magnetic resonance imaging have provided detailed information emerged regarding the vasoactive properties of these large vessels and how they may have significant impact on cerebral vascular conductance and flow. The overall conclusion is that conduit arteries do express dose-related vasoactive properties and contribute to global CBF reactivity, but in a manner that changes with age and vascular disease. 
Professor Kevin Shoemaker, University of Western Ontario, Canada

Professor Kevin Shoemaker, University of Western Ontario, CanadaDr Kevin Shoemaker is a Professor of Kinesiology and a Canada Research Chair in the Integrative Physiology of Exercise and Health in the Faculty of Health Sciences at the University of Western Ontario. His research emphasises the role of physical activity and exercise training in brain health, focusing on neurologic and vascular outcomes. Currently, he engages neuroimaging and microneurographic techniques to understand the cortical pathways and communication strategies used by the autonomic nervous system to affect homeostatic cardiovascular adjustments. His research also focuses on the cerebrovascular vulnerability to chronic inflammatory conditions, and its adaptability to exercise interventions. |
|
|---|---|---|
| 14:00 - 14:15 | Discussion | |
| 14:15 - 14:45 |
A neurostimulation therapy for disrupted neuro–cardiovascular control

Dr Aaron Phillips, University of Calgary, Canada

Dr Aaron Phillips, University of Calgary, CanadaDr Aaron Phillips research combines integrated physiology and neuroscience in order to understand cardiovascular function. Currently, the laboratory has two primary foci: the first is to understand the mechanisms underlying neurovascular regulation in the human brain; the second is to develop a neurostimulation therapy for restoring cardiovascular health in those with autonomic dysfunction. Aaron is currently collaborating with labs in Switzerland and Croatia as well as with clinicians in Minnesota to deeply understand the capacity of electrical stimulation of the spinal cord to control autonomic function. These studies are using murine models, as well as non-human primates and humans. |
|
| 14:45 - 15:00 | Discussion | |
| 15:00 - 15:30 | Tea | |
| 15:30 - 16:00 |
Integrated Control of Cerebral Blood Flow in Humans
No organ in the body is as dependent as the brain on steady supply of blood flow. Thus, the ability of cerebral vasculature to maintain stable blood flow in response to fluctuations in arterial gases and systemic blood pressure is critical to neural health. However, the utility of various experimental and analytic approaches to quantify cerebrovascular responses is still in dispute. Partly as a result, the nature and physiologic underpinnings of cerebrovascular control remain equivocal. For example, there is accumulating evidence for a role for autonomic nervous system in regulating cerebral blood flow. Moreover, recent evidence that autonomic neurogenic control may be responsible for homoeostatic maintenance of cerebral blood flow, and that myogenic control may be neuroprotective against ischaemia and haemorrhage from rapid swings in pressure. However, despite these data, specific aspects of this role remain unclear under debate. This talk will provide an overview of the recent work on different experimental and analytical approaches to understand cerebrovascular function, and on the impact of carbon dioxide–blood pressure interactions in shaping cerebral blood flow, with a particular emphasis on integrated neurogenic and regional control of the cerebral vasculature. 
Dr Can Ozan Tan, Harvard Medical School, Spaulding Rehabilitation Hospital, and Massachusetts General Hospital, USA

Dr Can Ozan Tan, Harvard Medical School, Spaulding Rehabilitation Hospital, and Massachusetts General Hospital, USADr Tan is an Assistant Professor at Harvard Medical School. He directs the Cerebrovascular Research Laboratory at Spaulding Rehabilitation Hospital, and holds an appointment at the Advanced X-ray Imaging Sciences (AXIS) Center and Division of Neuroradiology at Massachusetts General Hospital. His primary research area is human autonomic physiology, neuroimaging, and development of computational and statistical frameworks for clinical applications. His current research is focused on autonomic control of peripheral and cerebral circulation, the short- and long-term impact of traumatic and acquired brain injuries on cerebrovascular control and neural function, and the role of physical activity and aerobic exercise in neurorecovery. |
|
| 16:00 - 16:15 | Discussion | |
| 16:15 - 17:00 | Panel discussion/Overview (future directions) |

