Links to external sources may no longer work as intended. The content may not represent the latest thinking in this area or the Society’s current position on the topic.
Immuno-Oncology: How to get the immune system to beat cancer
This Royal Society conference explored immuno-oncology therapies - both current and recent technologies - whilst looking at removing barriers to their use.
Read the conference report summarising the event (PDF).
Background
Every two minutes, someone in the UK is diagnosed with cancer. Year on year, the cancer incidence rate continues to grow, with a projected increase of approximately 62% by 2040, resulting in over 27 million additional worldwide cancer cases per year. Traditionally, cancer has been treated using methods such as chemotherapy and radiotherapy. However, some cancers don’t respond well to traditional therapies, and others recur.
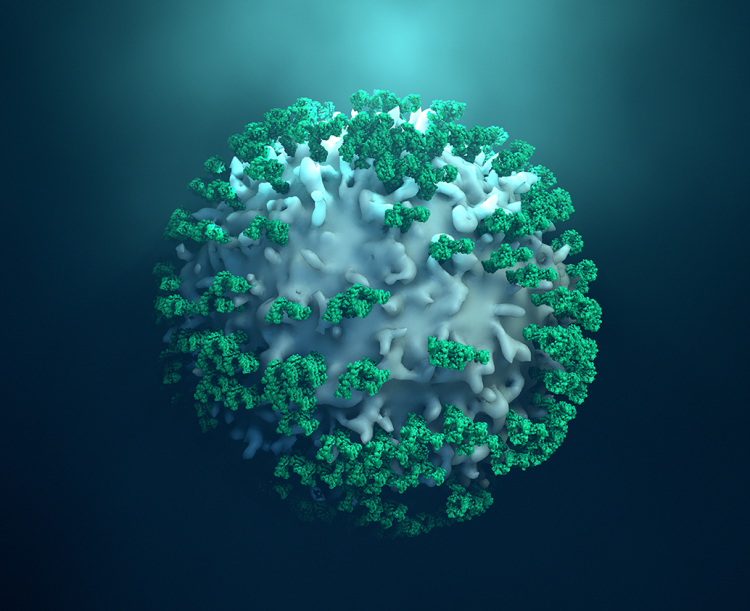
Immuno-oncology could help provide a solution to these problems by harnessing the body’s immune system to eradicate cancer and prevent its recurrence. Through combination therapy, and addressing the barriers to its use, immuno-oncology treatments could help tackle the rising number of worldwide cancer cases.
About the conference series
The conference is part of the Royal Society's Transforming our future conferences in the life sciences, supported by AstraZeneca. These meetings are unique, high-level events that address the scientific and technical challenges of the next decade. Each conference features cutting edge science from industry and academia and brings together leading experts from the scientific community, including regulatory, charity and funding bodies.
Organisers
Schedule
| 13:00 - 13:05 |
Welcome Remarks

Professor Dame Linda Partridge FMedSci FRS, Director, Institute of Healthy Ageing, University College London

Professor Dame Linda Partridge FMedSci FRS, Director, Institute of Healthy Ageing, University College LondonLinda Partridge works on the biology of ageing. Her research is directed to understanding the mechanisms by which healthy lifespan can be extended in laboratory model organisms and humans. Her work has focused in particular on the role of nutrient-sensing pathways, such as the insulin/insulin-like growth factor signalling pathway, and on the role of diet. She is the recipient of numerous awards, including the Royal Society's Croonian Prize Lecture, and was honoured with a DBE for Services to Science in 2009. She is a Fellow of the Royal Society, the Academy of Medical Sciences and a foreign member of the American Academy of Arts and Sciences. She is Director of the Institute of Healthy Ageing at UCL and the founding director of the Max Planck Institute for Biology of Ageing in Cologne, Germany. |
|---|
Chair

Dr Susan Galbraith FMedSci, SVP Early Oncology, AstraZeneca

Dr Susan Galbraith FMedSci, SVP Early Oncology, AstraZeneca
Susan Galbraith trained as a Clinical Oncologist in the United Kingdom. She studied Medicine at Manchester and Cambridge Universities. She has a PhD from the University of London involving translational work on a vascular-targeting agent. She has 20 years of industry cancer drug development experience, playing a key role in the development of several approved drugs including ipilimumab, nivolumab, olaparib, osimertinib, acalabrutinib and Selumetinib. She was awarded an honorary Doctorate of Medical Science from the Institute of Cancer Research in 2017, and was admitted to Fellowship of the Academy of Medical Sciences in 2018.
| 13:05 - 13:35 |
The Evolution of Immuno-oncology: An Industrial Perspective
With the advent of checkpoint inhibitors, immuno-oncology has experienced a remarkable renaissance, offering today an enlarged and relatively well tolerated spectrum of therapeutic options to patients. In particular, antagonists directed against the Programmed death-1 (PD-1) protein and its ligand are now widely used clinically, often in combination with appropriate biomarkers. However, whilst some patients exhibit full responses including remissions, some tumours don’t seem to respond satisfactorily or even not at all. The pharmaceutical industry is working intensely to identify combination partners of checkpoint-based backbone therapies as well as completely novel approaches in order to improve the robustness and durability of these treatments. The presentation will cover the key therapeutic modalities the industry is currently examining, highlighting their potential, limitations and recent successes. The importance of academic research as well as the dialogue between the industry and payors will also be highlighted. 
Dr Klaus Urbahns, Global Head of Discovery & Development Technologies, Healthcare R&D, Merck KGaA

Dr Klaus Urbahns, Global Head of Discovery & Development Technologies, Healthcare R&D, Merck KGaAKlaus Urbahns is head of Discovery & Development Technologies in Merck Healthcare’s R&D division. His laboratories are based in Darmstadt, Boston, Tel Aviv, Rome and Turin. Klaus is also serving on advisory roles for Malaria Ventures, the Lead Discovery Center (Max-Planck) and the Merck-Venture fund. He has been involved in immuno-oncology research and development for the last ten years. Prior to his role at Merck, Klaus has worked at AstraZeneca in the UK and Sweden and at Bayer in Germany and Japan. Klaus has studied at the Universities of Kiel and Freiburg and holds a Ph.D. in synthetic organic chemistry from the University of Frankfurt. |
|---|---|
| 13:35 - 14:05 |
Chromosomal instability and immune evasion in cancer evolution
TRACERx is a longitudinal cancer evolution study that aims to understand the interaction of complex evolving heterogeneous tumours with the tumour microenvironment across hundreds of patients. We have found that Chromosomal instability, is a major driver of intratumour heterogeneity contributing to parallel evolution, subclone selection and poor clinical outcome. The diversity of such tumour subclonal events in late stage tumours combined with tumour plasticity will likely confound the ability of monotherapy drugs targeting single clonal driver events to achieve sustained clinical benefit. We have found that tumour clonal neoantigens that may be recognized by cytotoxic T cells are major determinants of clinical outcome in treatment naïve and immune checkpoint inhibitor therapy treated patients, providing a therapeutic vulnerability in cancers with a high mutational burden. However, TRACERx has revealed multiple tumour adaptive mechanisms to immune predation, highlighting cancer chromosomal instability driving immune evasion through HLA class I and clonal neo-antigen loss as major routes to immune escape. How cancer genetic diversity limits an effective immune response and the role of clonal neoantigens as therapeutic targets to mitigate resistance and treatment failure will be discussed. 
Professor Charles Swanton FRS FMedSci, Translational Cancer Therapeutics Laboratory Group Leader, The Francis Crick Institute

Professor Charles Swanton FRS FMedSci, Translational Cancer Therapeutics Laboratory Group Leader, The Francis Crick InstituteDr Swanton completed his MD/PhD in 1999 at the Imperial Cancer Research Fund Laboratories and Cancer Research UK clinician/scientist medical oncology training in 2008. He combines his laboratory research at the Francis Crick Institute with clinical duties focused on biological mechanisms of cancer drug resistance. Dr Swanton was made Fellow of the Royal College of Physicians in April 2011 and Chair in Personalized Cancer Medicine and Consultant Thoracic Medical Oncologist at UCL Hospitals in November 2011. Dr Swanton is the Chief Investigator of the CRUK TRACERx lung cancer evolution study and was awarded the Royal College of Physicians Goulstonian lecture and Graham Bull Prize for Clinical Sciences in 2013, Fellow of the European Academy of Cancer Sciences in 2013, and Fellow of the Academy of Medical Sciences in 2015. Dr Swanton was awarded the Jeremy Jass Prize (2014), Stand up to Cancer Translational Cancer Research Prize (2015), Glaxo SmithKline Biochemical Society Prize in recognition of distinguished research leading to new advances in medical science and the Ellison-Cliffe Medal and Lecture, Royal Society of Medicine (2016). He was appointed Napier Professor in Cancer by the Royal Society in 2016, Cancer Research UK’s Chief Clinician in 2017. He was awarded the 2016 San Salvatore Foundation prize, and elected an EMBO member in 2017. |
Chair

Dr Susan Galbraith FMedSci, SVP Early Oncology, AstraZeneca

Dr Susan Galbraith FMedSci, SVP Early Oncology, AstraZeneca
Susan Galbraith trained as a Clinical Oncologist in the United Kingdom. She studied Medicine at Manchester and Cambridge Universities. She has a PhD from the University of London involving translational work on a vascular-targeting agent. She has 20 years of industry cancer drug development experience, playing a key role in the development of several approved drugs including ipilimumab, nivolumab, olaparib, osimertinib, acalabrutinib and Selumetinib. She was awarded an honorary Doctorate of Medical Science from the Institute of Cancer Research in 2017, and was admitted to Fellowship of the Academy of Medical Sciences in 2018.
| 14:20 - 14:45 |
Programming cells through genetic engineering – Advancing cell therapy innovation
Autologous T-cell therapies are now on the market and many more innovative T-cell products are in pre-clinical or clinical trials to treat a wide range of cancer patients. The recent explosion in cell modification techniques, through viral vectors and specific genetic editing, coupled with the ever-expanding knowledge of the human genome, provides a powerful toolkit for drug developers to improve on current therapies. Arming cells with receptors to enable them to recognise tumours efficiently, as well as adapting them to traffic to tumours more effectively and overcome resistance mechanisms, can generate improved products. A key factor for these treatments is understanding the cells themselves. The move from individual patient manufacturing towards “off-the-shelf” allogeneic alternatives should enable deeper product understanding and greater consistency. When multiple patients can be treated with the same batch of cells, from healthy donors or differentiated stem cells, it is possible to iterate product design based on translational data without the confounding factor of variable starting material – which will be an important step forward in the constant search for higher response rates and ultimately cures. 
Jo Brewer, SVP Allogeneic Research, Adaptimmune Ltd.

Jo Brewer, SVP Allogeneic Research, Adaptimmune Ltd.Dr Jo Brewer has served as Senior Vice President, Allogeneic Research since December 2019. She leads Adaptimmune’s efforts to generate new, off-the-shelf, cell therapies for people with cancer, as well as developing the manufacturing processes for these therapies. Jo has more than 19 years of experience in immunotherapy research, specifically preclinical development of assets from the early research phase towards first-in-human trials. She was one of the founding scientists at Adaptimmune, working on the early SPEAR T-cell programs. She built multiple research teams over 11 years aimed at improving the efficacy of SPEAR T-cell therapies through translational learning leading to the development of multiple next-gen approaches, the first of which is being tested in the SURPASS trial. Dr Brewer holds a MA and PhD from the University of Cambridge. |
|---|---|
| 14:45 - 15:10 |
Manufacture and delivery of cell therapies

Dr Stanley Frankel, Associate Professor of Medicine, Columbia University Vagelos College of Physicians and Surgeons

Dr Stanley Frankel, Associate Professor of Medicine, Columbia University Vagelos College of Physicians and SurgeonsDr. Stan Frankel is hematologist/oncologist who focuses on drug development and clinical trials. He consults to the biopharma industry and investors. Stan received his B.A. from Harvard College and his M.D. from Northwestern University. He received his post-graduate training at Mount Sinai Hospital in New York, and Memorial Sloan-Kettering Cancer Center where he was Chief Fellow. He had an academic practice in stem cell transplantation and hematologic malignancy clinical trials at Roswell Park Cancer Center, Georgetown University and the University of Maryland. Dr. Frankel is a Diplomate of the American Board of Internal Medicine with subspecialty credentials in Hematology and Medical Oncology. He is also an Adjunct Associate Professor of Medicine at the Vagelos College of Physicians and Surgeons at Columbia University and licensed to practice in New York. He is a Fellow of the American College of Physicians. He is a member of ACP, AACR, ASTCT, ASCO, ASH, EHA, and ESMO. He has authored more than 80 peer-reviewed scientific papers. |
| 15:10 - 15:35 |
CAR-T cell therapy in the clinic: lessons learned and road ahead
T cell genetically modified to express chimeric antigen receptor (CAR-T cells) are a radically innovative way for tackling cancer. CAR-T cells have demonstrated unprecedented curative potential in diseases such as pediatric acute lymphoblastic leukaemia, non-Hodgkin lymphoma and multiple myeloma. The talk will focus on the science behind CAR-T cells, the determinants driving therapeutic efficacy and on aspects related to manufacturing and supply. Moreover, recognized gaps for translating CAR-T successes to solid tumours will be discussed. 
Dr Attilio Bondanza, Head of Clinical Development, Cell Therapy Unit, Oncology R&D, AstraZeneca

Dr Attilio Bondanza, Head of Clinical Development, Cell Therapy Unit, Oncology R&D, AstraZenecaAttilio Bondanza is Head of Cell Therapy Clinical at Astrazeneca Oncology R&D in Cambridge UK. Prior to that, he was Senior Global Program Leader at Novartis Basel CH, where he contributed to the clinical development of tisagenlecleucel (Kymriah), the first CAR-T cell therapy approved in the US, and initiated several other new CAR-T cell programs. Before joining the industry, Attilio was Associate Professor at the San Raffaele University of Milano IT. He is board-certified in Internal Medicine and holds a PhD in Transplantation Immunology. He has an H-index of 36 and is the inventor of several granted patents in the field of CAR-T cell therapy. |
Chair

Professor Luke O'Neill FRS, Chair of Biochemistry, Trinity College Dublin

Professor Luke O'Neill FRS, Chair of Biochemistry, Trinity College Dublin
Luke O’Neill is Professor of Biochemistry in the School of Biochemistry and Immunology, Trinity Biomedical Sciences Institute at Trinity College Dublin, Ireland. He is a world expert on innate immunity and inflammation. His main research interests include Toll-like receptors, Inflammasomes and Immunometabolism. He is listed by Thompson Reuters/ Clarivates in the top 1% of immunologists in the world, based on citations per paper.
| 15:50 - 16:15 |
The role of the gut and tumor microbiome in cancer
We have made major progress in the treatment of cancer: however, responses to cancer treatment are heterogenous and not always durable. There is a growing appreciation of factors impacting carcinogensis and canner therapy response, with the microbiome taking center stage. Within our bodies, we have trillions of microbes that may outnumber our own normal cells – and these microbes and their genomes (collectively referred to as the microbiome) can profoundly impact our physiology. The microbiome and its relationship to cancer will be discussed, including the tumor and gut microbiome. 
Dr Jennifer Wargo, Professor, Department of Genomic Medicine, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center

Dr Jennifer Wargo, Professor, Department of Genomic Medicine, Division of Cancer Medicine, The University of Texas MD Anderson Cancer CenterProfessor Wargo’s career commitment is to advance the understanding and treatment of disease through science. In September 2013, Dr Wargo joined the University of Texas MD Anderson Cancer Center after being recruited from Massachusetts General Hospital/Harvard Medical School where she obtained her medical degree and completed two fellowships at the University of California and NIH in Surgical Oncology. Dr Wargo holds joint appointments in Surgical Oncology as a Melanoma surgeon and Genomic Medicine conducting her critical research in the field of microbiome and translational research. In 2019, Dr Wargo started a microbiome and translational research program at MD Anderson Cancer Center called PRIME TR “Program for Innovative Microbiome and Translational Research”. |
|---|---|
| 16:15 - 16:40 |
Using genomics for the design and response monitoring of personalized cancer vaccines
In addition to its role in identifying cancer drivers that may be predictive of response to targeted therapies, genomic characterization of individual cancers provides a data set to identify potential neoantigens and predict their binding affinity for class I and class II MHC. Our efforts to produce a computational pipeline and tool set for these purposes will be described along with current data obtained from their use to characterize GBM samples from an accruing clinical trial of DNA-based personalized neoantigen vaccines. In addition, the use of genomics-based methods to evaluate immune responses post-infusion will be outlined. 
Dr Elaine Mardis, co-Executive Director of the Steve and Cindy Rasmussen Institute for Genomic Medicine, Nationwide Children's Hospital

Dr Elaine Mardis, co-Executive Director of the Steve and Cindy Rasmussen Institute for Genomic Medicine, Nationwide Children's HospitalElaine Mardis, PhD is co-Executive Director of the Steve and Cindy Rasmussen Institute for Genomic Medicine at Nationwide Children’s Hospital and holds the Rasmussen Nationwide Foundation Endowed Chair of Genomic Medicine. She also is Professor of Pediatrics at The Ohio State University College of Medicine. Educated at the University of Oklahoma with a BS in Zoology and a PhD in Chemistry and Biochemistry, Dr Mardis did postgraduate work in industry at BioRad Laboratories. She was a member of the faculty of Washington University School of Medicine from 1993-2016. Dr Mardis has authored over 380 articles in peer-reviewed journals and has been listed since 2013 as one of the most highly cited researchers in the world by Thompson Reuters. Dr Mardis was given the Morton K. Schwartz award from the American Association for Clinical Chemistry in 2016 and the Heath Memorial Award from MD Anderson Cancer Center in 2020. Dr Mardis is the Immediate Past AACR President. She was elected a Fellow of the AACR Academy, and was elected to membership in the National Academy of Medicine in 2019. |
| 16:40 - 17:05 |
Oncolytic immuno-virotherapy: promises, technical barriers, and recent progresses
The approval of talimogene laherparepvec, and the large number of clinical trials with encouraging intermediate results should not make us forget the major challenges to install oncolytic viruses (OVs) as a new recognized therapeutic class. These clinical developments have highlighted the key features for potent OV candidates, and also some specific properties requested for some applications. The ability to deliver large recombinant payloads into the tumor, i.e. armed OVs, is one of them as it provides additional therapeutic levers such as local activation of effector cells, blockade of immunosuppressive pathways, or metabolic modifications. In parallel, current research aims at overcoming the major obstacles encountered by OVs in their mode of action. These barriers might both be biological and physical. We will share some lessons learned from the development of Vaccinia-based oncolytic products, and some recent progresses in virus bioengineering or in delivery techniques that have raised optimism. 
Dr Eric Quemeneur, Executive Vice President, and Chief Scientific Officer, Transgene

Dr Eric Quemeneur, Executive Vice President, and Chief Scientific Officer, TransgeneDr Eric Quemeneur is a biochemist (PhD 1989, HDR 1999) and industrial pharmacist (PharmD 1988). His scientific and professional experience have developed in the fields of protein engineering, toxicology, and more recently immunotherapy and virology. He joined Transgene at the end of 2014 to renovate the company’s product and technology portfolio, and to boost its open innovation policy. Major achievements have been the launch of the invirIO™ platform for armed oncolytic viruses, the myVAC™ program for personalized neoantigen-based cancer vaccines, and key strategic partnerships with major pharma or AI companies. Prior to Transgene, he held various research direction positions at the CEA Life Sciences Division, French Army Health Service, Biomerieux, and Hoechst A.G. |
Chair

Professor Sir Roy Anderson FMedSci FRS, Professor of Infectious Disease Epidemiology, Imperial College London

Professor Sir Roy Anderson FMedSci FRS, Professor of Infectious Disease Epidemiology, Imperial College London
Sir Roy is currently Professor of Infectious Disease Epidemiology in the School of Public Health, Faculty of Medicine, Imperial College London and Director of the London Centre for Neglected Tropical Disease Research. His past posts include, the Chief Scientist at The UK Ministry of Defence, and Rector of Imperial College London. He is the author of over 650 scientific articles and has an h index of 133 in google scholar.
Among many past commitments, he served as a Trustee of the Natural History Museum London, and as a non-executive director of GlaxoSmithKline for ten years. He is currently Chair of Oriole Global Health Ltd, a Vice President of Fauna and Flora International, Trustee of the London Institute of Mathematical Sciences and of the Banga charity.
Sir Roy was elected Fellow of the Royal Society in 1986, a Founding Fellow of the Academy of Medical Sciences in 1998, and a Foreign Associate Member of both the National Academy of Medicine at the US National Academy of Sciences in 1999 and of the French Academy of Sciences in 2010. He was knighted in the 2006 Queen's Birthday Honours.
| 13:45 - 14:10 |
Artificial intelligence for digital tissue biomarker discovery in immuno-oncology
Artificial Intelligence (AI) systems have surpassed human intelligence, fueled by the availability of dedicated high performance hardware, sophisticated deep learning architectures and algorithms, and Big Data. Deep convolutional neural networks have been successfully used to generate quantitative insights into the cancer immune contexture, and to replicate pathologists diagnostic scoring of tissue slides. However, the discovery of predictive biomarkers for immuno-oncology using computational pathology remains challenging. Standard fully supervised deep learning methods require extensive training data from expert pathologists. Latest weakly supervised methods aim towards superhuman performance, but frequently lack interpretability and transparency. Although regulatory authorities such as the FDA are increasingly open to approve AI "software as a medical device" systems, no histopathology-based companion diagnostic test has been yet marketed. The recent CE marks for prostate and breast cancer detection by AI-based clinical grade systems are promising milestones towards a wider adoption of computational pathology in the clinical routine, for the benefit of our patients. 
Dr Günter Schmidt, Vice President, Image Data Science, AstraZeneca

Dr Günter Schmidt, Vice President, Image Data Science, AstraZenecaDr Guenter Schmidt, Vice President Image Data Sciences, joined AstraZeneca Computational Pathology GmbH in 1995. He worked with Nobel laureate Professor Dr Gerd Binnig on the invention of the Artificial Intelligence (AI) platform Cognition Network Technology and its application to contextual image and data understanding software, and based on that, to decision support systems. Today, Guenter’s AI research, image analysis and data science teams work within oncology drug development and biomarker programs, driving the development and application of robust and scalable state of the art deep learning solutions to investigate mechanisms of action (MoA) and to discover predictive biomarkers. Guenter is a computational nuclear physicist with a doctorate degree from the Eberhard-Karls University of Tübingen, Germany. |
|---|---|
| 14:10 - 14:35 |
Employing novel technologies to improve immunotherapy
Immunotherapy has significantly improved the outlook of patients with cancer. Early studies have shown benefit of check point inhibitors in metastatic cancer and now neoadjuvant immunotherapy has shown the curative potential of this treatment. However, the majority of patients do not have benefit of this treatment and studies to better understand mechanisms of resistance or allow better patient selection are highly needed. We have employed preclinical models to better understand the interaction between cancer cells and the immune system. These models provide new insights and pave the way to individualized immunotherapy. 
Professor Emile Voest, Netherlands Cancer Institute, The Netherlands

Professor Emile Voest, Netherlands Cancer Institute, The NetherlandsEmile Voest is medical oncologist, senior group leader at the Netherlands Cancer Institute, senior scientist of the Oncode Institute, and translational scientist. He is the current director of Cancer Core Europe, a collaboration of 7 excellent comprehensive cancer centers. His laboratory group is devoted to bringing precision medicine to patients and is focused on mechanistic studies of tumor biology and applying computational science and genomics to better understand how tumors respond to certain treatments. The results from these studies are subsequently tested for their value in patients. These translational approaches are performed across tumor types with emphasis on epithelial tumors. His research is in the area of precision medicine and consists of large scale genomic sequencing of patients with metastatic cancer, the development of primary cultures of tumors for ex vivo testing (including tumor organoids) and the use of these cultures to improve drug development and to determine which treatment is best for a specific patient. |
| 14:35 - 15:00 |
Tumor Re-Engineering: Developing Novel Immuno-Gene Therapies for Cancer
Combining different anti-cancer immunotherapeutics is currently a major focus of clinical oncology studies, but while this can increase efficacy this benefit usually comes at a price of increased, dose limiting toxicity. Because these agents are dosed systemically, they frequently cause unwanted immune inflammation in a variety of organ systems as well as in the intended tumor lesions. Tumor re-engineering aims to overcome these issues by enabling selective delivery to and/or production of the therapeutic agent or combinations in tumor tissues where they are needed while minimizing systemic exposure. We are developing a tumor-specific immune-gene (T-SIGn) vector approach that delivers biotherapeutic gene payloads for production by the tumor cells themselves. These aim to promote anti-tumor immunity from within the lesions by targeting elements of the tumor and local lymphoid microenvironments. This presentation will use data generated with different clinical and preclinical stage T-SIGn candidates to illustrate these concepts. 
Dr Brian Champion, Chief Scientific Officer, PsiOxus Therapeutics

Dr Brian Champion, Chief Scientific Officer, PsiOxus TherapeuticsDr Brian Champion is Chief Scientific Officer and member of the Executive Management Team at PsiOxus Therapeutics Ltd, Oxford, UK where he is leading the scientific team in the development of novel oncolytic virus-based, Tumor-Specific Immunogene (T-SIGn) therapies for the treatment of cancer. He was previously Executive Director and Head of Immunology for Pfizer's Vaccine Immunotherapeutics Research Unit in La Jolla, California, leading the immunology team providing expertise and immunoassays for Pfizer vaccine projects, program leader for an anti-IgE therapeutic vaccine for allergy/asthma, and a member of the leadership team. Prior to this he was Site Head for Pfizer Vaccine Research in the UK. Before joining Pfizer, Dr Champion was Chief Scientific Officer for Lorantis and Celldex in Cambridge (UK) developing protein and DNA-based, antigen-specific immunotherapeutic approaches to a variety of immunological diseases, including therapeutic vaccines and immunotherapeutic biomolecule approaches for cancer, infectious diseases, allergies and autoimmune disorders. Prior to Lorantis, he was with Glaxo and GlaxoWellcome (UK and USA) for 13 years, focusing primarily on target discovery and validation research for autoimmune, allergic and bone disorders. |

Dr Stuart Farrow, Director of Biology, Cancer Research UK Therapeutic Discovery Laboratory

Dr Stuart Farrow, Director of Biology, Cancer Research UK Therapeutic Discovery LaboratoryBefore joining Cancer Research UK Therapeutic Discovery laboratories as director of biology in 2015, Stuart spent more than 20 years in drug discovery and leadership roles in the pharmaceutical industry. Most recently he was based at the University of Manchester, where he directed the establishment of the Manchester Centre for Collaborative Research in Inflammation (MCCIR), a £15M initiative funded by GlaxoSmithKline, AstraZeneca and the University of Manchester. He is a past member of the MRC Infection and Immunity Board. Stuart has worked in several therapeutic areas and has directed major translational research initiatives in apoptosis, immunology and circadian biology. He has led discovery teams that have generated several clinical candidate molecules and has overseen biology programmes for drugs that have achieved regulatory approval and launch. In his current role he has been closely involved in the establishment of major drug discovery alliances in cancer immunology between CR-UK and various industry partners. 
Dr Jacqueline Barry, Chief Clinical Officer, Cell and Gene Therapy Catapult

Dr Jacqueline Barry, Chief Clinical Officer, Cell and Gene Therapy CatapultJacqueline Barry is the Chief Clinical Officer, responsible for Clinical Translation and Delivery activities and an Executive Director of the Cell and Gene Therapy Catapult. She has extensive experience in the development of advanced therapy medicinal products and leads a multi-disciplinary team of Nonclinical, Regulatory, Clinical Operations and Programme Management specialists. She also leads the coordination of the UK Advanced Therapy Treatment Centre Network and is a Director of the Global Alliance for iPSC Therapies. She feels passionately about making advanced therapies available for patients and works closely with the MHRA and the NHS on the development of the ecosystems to support the adoption of these therapies. Prior her time at Cell and Gene Therapy Catapult, Jacqueline worked at the Scottish National Blood Transfusion Service where amongst other activities she designed the regulatory strategy for the Cellular Therapies for the Blood Transfusion Service and acted as Qualified Person for their release. She has a PhD from the University of Aberdeen and did post-doctoral research in neurophysiology at the University of Edinburgh. 
Professor Fiona Thistlethwaite, Medical Oncology Consultant, The Christie NHS Foundation Trust
Professor Fiona Thistlethwaite, Medical Oncology Consultant, The Christie NHS Foundation Trust |
| 16:30 - 17:00 |
Cancer Immunotherapy: Today's Triumphs and Tomorrow's Treatments
Cancer cells induce a set of adaptive response pathways to survive in the face of stressors due to inadequate nutrient supply. One such adaptive pathway is the unfolded protein (UPR) or endoplasmic reticulum (ER) stress response mediated in part by the ER-localized transmembrane sensor IRE1 and its substrate XBP1. XBP1 promotes intrinsic tumor growth directly in the setting of triple negative breast cancer and also regulates the host anti-tumor immune response. A hostile tumor microenvironment (TME) composed of adaptive and innate immune cells that secrete or express immunosuppressive substances is one of the major barriers to achieving T cell-mediated tumor lysis. Reprogramming these immune cells through silencing the ER stress response reprograms a hostile TME to initiate and sustain T cell-dependent anti-cancer immunity. Targeting the ER stress response should concomitantly inhibit tumor growth and enhance anti-cancer immunity, thus offering a unique approach to cancer immunotherapy. 
Dr Laurie Glimcher, President and CEO, Dana-Farber Cancer Institute

Dr Laurie Glimcher, President and CEO, Dana-Farber Cancer InstituteLaurie H. Glimcher, MD is the President and CEO of the Dana-Farber Cancer Institute, Director of the Dana-Farber/Harvard Cancer Center and the Richard and Susan Smith Professor of Medicine at Harvard Medical School. She is a Member of the National Academy of Sciences, the National Academy of Medicine and the American Philosophical Society, Fellow of the American Academy of Arts and Sciences and the former President of the American Association of Immunologists. She served on the Vice President’s Blue Ribbon panel. She currently serves on the Board of Directors of GlaxoSmithKline Pharmaceutical Corporation and Analog Devices, Inc. Dr Glimcher’s research identified key transcriptional regulators of protective immunity and the origin of pathophysiologic immune responses underlying autoimmune, infectious and malignant diseases. Aside from her research efforts, Dr Glimcher has been a staunch proponent of improved access to care, health policy, and medical education, while simultaneously serving as a pioneering mentor and role model for cancer research trainees and for all women in science. |
|---|
