Evaluating anti-infective drugs
Theo Murphy meeting organised by Dr James Watson, Dr William Schilling and Professor Nicholas White.
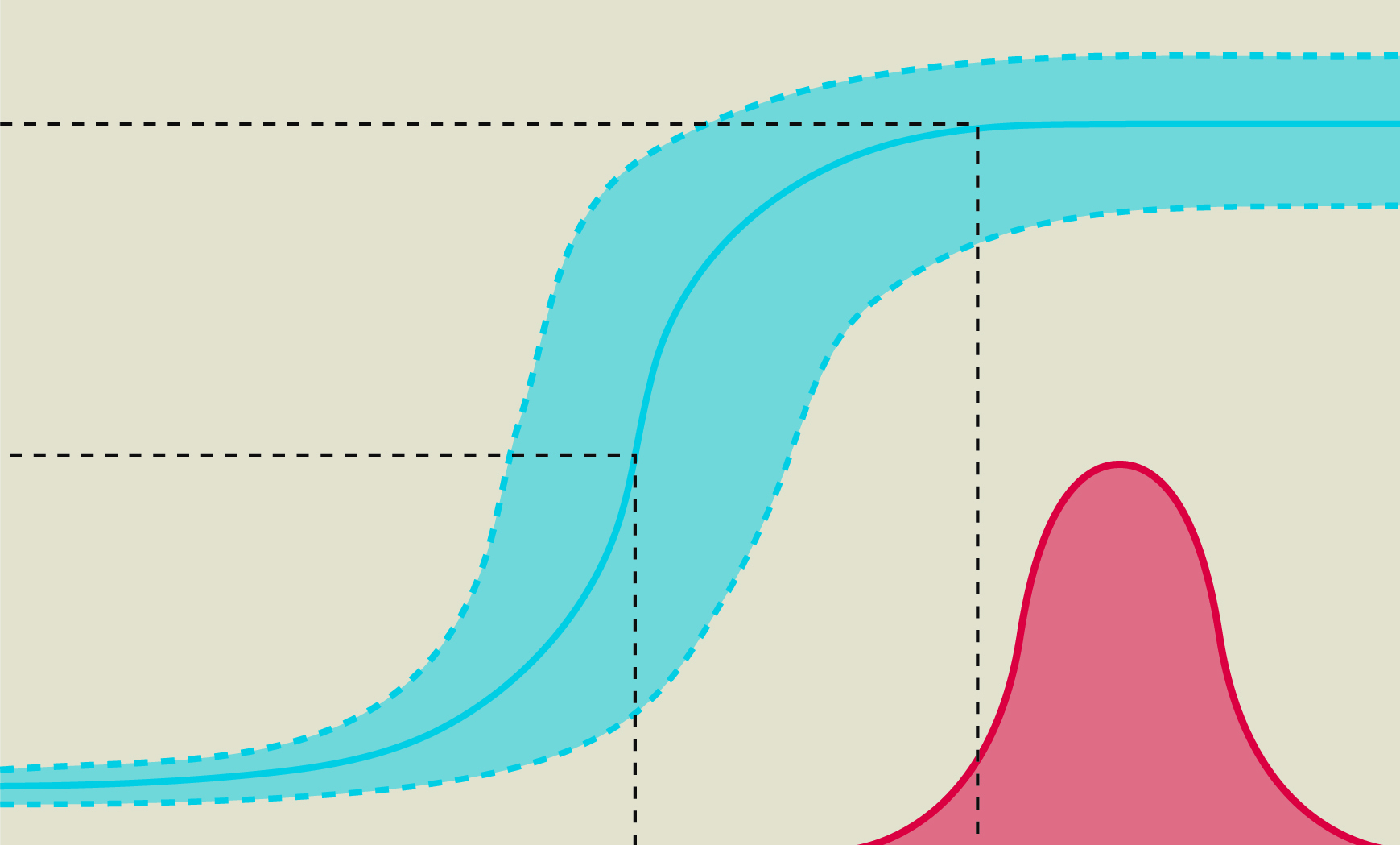
Our objective is to draw upon experience and evidence across infectious diseases to derive common principles and approaches to in-vivo pharmacodynamic assessment and to discuss the optimal design, evaluation and interpretation of pharmacometric studies. We will compare the pharmacometric approaches and methodologies used across major infectious diseases to inform the development and rapid assessment of interventions for future pandemics.
Attending the meeting
This event was intended for researchers in relevant fields, and was a residential meeting taking place at the Midland Hotel, Manchester.
- Free to attend
- Advance registration essential
- This was an in-person only meeting
Enquiries: contact the Scientific Programmes team.
Organisers
Schedule
Chair

Professor Julie Anne Simpson, University of Melbourne, Australia

Professor Julie Anne Simpson, University of Melbourne, Australia
Professor Julie Simpson is Head of Biostatistics at the Melbourne School of Population and Global Health and Director of the Methods and Implementation Support for Clinical and Health research (MISCH) Hub at the University of Melbourne, and a Visiting Professor of the University of Oxford. She has 30 years’ experience collaborating on multidisciplinary research projects with clinicians, laboratory scientists, epidemiologists and health policy-makers at universities and hospitals worldwide, and has published >370 papers. Her main area of research is the integration of biostatistics and mathematical modelling to improve the control of infectious diseases.
| 09:00-09:05 |
Welcome by the lead organiser

Dr James Watson, University of Oxford, UK

Dr James Watson, University of Oxford, UKJames Watson is a statistician and the Associate Director at the Infectious Diseases Data Observatory, a data re-use platform aimed at helping improve the treatment of major infectious diseases. His main work focuses on severe malaria, notably improving the definition of severe malaria in areas of high malaria transmission. He helped develop the statistical methodology for adaptive platform trials characterising antiviral effects of therapeutics in SARS-CoV-2, influenza, RSV, and dengue. He is an investigator on the CHARM project, which aims to develop a new methodology for the assessment of new antiparasitic drugs for the treatment of Chagas disease. |
|---|---|
| 09:05-09:30 |
Malaria
Malaria is the most important parasite of man. Most deaths from falciparum malaria (estimated 2000 per day) occur in African children. Malaria disease results from the proliferation of intraerythrocytic Plasmodium parasites. The first symptoms of illness (fever) occur when the number of parasites in the blood reaches about 2 million/ kg. This corresponds with about 1 parasite per 200 white cells in a thick blood smear. Mortality rises when parasite burdens exceed 2 x 1010/ kg (corresponding to about 2% parasitaemia), although the relationship between intravascular parasite burden and parasite density in the peripheral blood smear is confounded by the sequestration of erythrocytes containing mature forms of the asexual parasites in the deep vasculature. The initial multiplication of malaria parasites in people with no immunity approximates 10 fold per asexual cycle (which is 48 hours in P. falciparum and P.vivax), but this stops abruptly at high densities. Antimalarial drugs which accelerate ring stage clearance can be readily assessed by measurement of parasite clearance rates. Intra-host modelling can also be used to assess in-vivo inhibitory concentrations and assess therapeutic responses. Simple pharmacometric models explain most aspects of the therapeutic response in malaria and can be used to optimise treatment regimens. Professor Nick White FRS, Mahidol Oxford Research Unit
Professor Nick White FRS, Mahidol Oxford Research UnitProfessor Nick White is Professor of Tropical Medicine at the Faculty of Tropical Medicine, Mahidol University, Thailand and Oxford University, UK. He is a Wellcome Trust Principal Research Fellow who chairs the Wellcome Trust Tropical Medicine Research Programmes in South East Asia. His main research focus is the pathophysiology and treatment of malaria. He also currently conducts pharmacometric research on COVID-19, influenza, and Chagas disease. Professor White has received the Prince Mahidol Prize for Medicine, the Canada Gairdner Foundation Global Health Prize, and the Royal Society of Tropical Medicine and Hygiene Manson medal. He has been a member of the WHO antimalarial treatment guidelines committee for 20 years (and co-chaired it for twelve) and he currently chairs the Scientific Advisory Committee of the Drugs for Neglected Diseases initiative and the Coalition for Equitable Research in Low Resource Settings. |
| 09:30-09:45 |
Discussion
|
| 09:45-10:15 |
The application of clearance markers in clinical trials of fungal infections
Invasive candidiasis and cryptococcal meningitis are the most common invasive fungal infections globally, affecting patients in the ICU and with advanced HIV respectively. Early fungicidal activity (EFA), a continuous measure of fungal clearance from serial samples of cerebrospinal fluid- was first implemented by our research group in clinical trials in the early 2000s and has now been widely adopted as an endpoint in phase II and III trials of cryptococcal meningitis. The task is more challenging in other mycoses, including invasive candidiasis/ candidaemia, where the evaluation of novel antifungals in the pipeline has been hampered by the lack of treatment response biomarkers. Preliminary data on beta-D glucan (fungal cell wall antigen) clearance kinetics from an ongoing observational study in candidaemia will be presented for discussion. 
Professor Tihana BicanicCity St George's University of London, UK 
Professor Tihana BicanicCity St George's University of London, UK Tihana Bicanic is an Infectious Diseases Physician at St George’s University and Hospital in London, with a specialist interest in management of Invasive fungal infections. She has specific experience in the implementation and evaluation of fungal clearance in clinical trials in cryptococcal meningitis- and more recently, candidaemia. |
| 10:15-10:30 |
Discussion
|
| 10:30-11:00 |
Break
|
| 11:30-11:45 |
Discussion
|
| 11:45-12:15 |
HIV
Professor Saye H Khoo, University of Liverpool, UK
Professor Saye H Khoo, University of Liverpool, UKProfessor Saye Khoo is Professor in Infection Pharmacology at the University of Liverpool, and Honorary Consultant Physician in Infectious Diseases at the Royal Liverpool University Hospital. Current research includes clinical trials of antimicrobials, characterisation of drug-drug interactions involving antiviral agents, and pharmacology of anti-infective agents. Khoo leads the UK Early-Phase COVID-19 Antiviral Trials Platform (AGILE) for experimental antivirals, and is Chief Investigator of the international DolPHIN consortium undertaking RCTs to establish safety and efficacy of HIV antivirals in pregnant women and their infants. He also leads the Liverpool Drug Interactions programme which has developed prescribing tools for managing drug interactions in HIV, hepatitis, and COVID-19 treatments. Collectively the tools returned over 16 million searches in 2023, and have been translated into Spanish, Portuguese and Japanese. Khoo has established the Liverpool Bioanalytical Facility, which undertakes GCP measurement of drug concentrations in plasma, cells, and tissue compartments. |
| 12:15-12:30 |
Discussion
|
| 13:30-14:00 |
Global challenges in antimicrobial therapy and AMR
Professor William Hope OBE, University of Liverpool, UK
Professor William Hope OBE, University of Liverpool, UKProfessor William Hope OBE (BMBS, FRACP, FRCPA, PhD), is the Dame Sally Davies Chair of AMR Research at the University of Liverpool in the UK. Professor Hope is a Fellow of the Royal Australasian College of Physicians and a Fellow of the Royal College of Pathologists of Australasia. Professor Hope qualified in Medicine in 1991, before undertaking specialist training in infectious diseases and clinical microbiology. He completed his PhD in antimicrobial pharmacology in 2006, while undertaking fellowships at the University of Manchester, UK, and the National Institutes of Health, Bethesda, USA. He was an NIHR Clinician Scientist and this award focused on individualised antimicrobial therapy. Areas of special interest and research are antimicrobial pharmacokinetics and pharmacodynamics, antimicrobial drug development and individualisation of antimicrobial therapy. He is a Fellow of the American Academy of Microbiology and European Society of Clinical Microbiology and Infectious Diseases. |
Chair

Dr James Watson, University of Oxford, UK

Dr James Watson, University of Oxford, UK
James Watson is a statistician and the Associate Director at the Infectious Diseases Data Observatory, a data re-use platform aimed at helping improve the treatment of major infectious diseases. His main work focuses on severe malaria, notably improving the definition of severe malaria in areas of high malaria transmission. He helped develop the statistical methodology for adaptive platform trials characterising antiviral effects of therapeutics in SARS-CoV-2, influenza, RSV, and dengue. He is an investigator on the CHARM project, which aims to develop a new methodology for the assessment of new antiparasitic drugs for the treatment of Chagas disease.
| 13:30-14:00 |
Modelling to support drug repurposing against hemorrhagic fever viruses
Jeremie will discuss the use of models to optimise drug repurposing against Ebola, Lassa, and Nipah viruses. He will specifically focus on the use of experimental animal models and translation to humans. The talk will also discuss recent similar developments in the context of mpox infection. 
Jeremie Guedj, French National Institute of Health and Medical Research, France

Jeremie Guedj, French National Institute of Health and Medical Research, FranceJeremie is a research scientist in biostatistics/ pharmacometrics at the French Institute of Health & Medical Research (INSERM), specialised in infectious diseases and antiviral treatment. His researches have theoretical objectives, such as developing mathematical models to understand quantitative aspects of host/ pathogen interaction. They also aim to impact clinical research by optimising drug combination, dosing regimen and identify characteristics associated with a differential response to antiviral treatment, in chronic (HIV, HBV, HCV) or acute viral infections (SARS-CoV-2, Ebola). He works in the IAME laboratory devoted to infectious diseases, and located on the premises of Hospital Bichat campus, in the north of Paris. He is leading a group of pharmacometrics, biostatistics, and clinical investigation in infectious diseases of about 30 young scientists (Master & PhD students, Postdocs) and tenured scientists. |
|---|---|
| 14:00-14:15 |
Discussion
|
| 14:15-14:45 |
Treatment of influenza
This talk will cover antiviral agents and immune-modulating agents in treating influenza. 
Professor David S Hui, The Chinese University of Hong Kong, Hong Kong
Professor David S Hui, The Chinese University of Hong Kong, Hong KongDavid Hui is the Chairman of Department of Medicine and Therapeutics and the Stanley Ho Professor of Respiratory Medicine, The Chinese University of Hong Kong (CUHK). He has joined the CUHK as an academic clinician since 1998 and is based at the Prince of Wales Hospital, HK where a major outbreak of SARS occurred in 2003. Since 2004, he has frequently served as an advisor to the WHO on the clinical management of emerging severe acute respiratory infections (SARI) including avian influenza, pandemic influenza, MERS and recently COVID-19. He also joined urgent WHO missions for the investigation of MERS nosocomial outbreaks in Riyadh and South Korea in 2013 and 2015 respectively. He has been rated as the top 1% highly cited researcher from 2021 to 2023 by Clarivate. |
| 14:45-15:00 |
Discussion
|
| 15:00-15:30 |
Break
|
| 15:30-16:00 |
Dengue nonstructural protein 1 as a surrogate marker: enhancing evaluation of antiviral efficacy alongside viremia levels
Dengue virus (DENV) infection remains a significant global public health challenge. Currently, no effective antiviral drug exists for DENV, and available vaccines show inconsistent efficacy across all four serotypes, with concerns about antibody-dependent enhancement in seronegative recipients. As such, developing antiviral treatments remains a critical need. In early-phase clinical trials, virological efficacy is typically assessed by measuring reduction in viremia levels and time to viremia clearance, which indicate effective drug action. However, symptomatic dengue patients generally seek medical care when viremia is already in decline, limiting the window for drug administration and complicating efficacy assessment. Furthermore, viremia often becomes undetectable within days without any intervention. Nonstructural protein 1 (NS1), which correlates with both viremia and disease severity, offers a complementary marker. NS1 remains detectable after viremia clearance, reflecting ongoing viral replication in infected cells, and has been shown to exert direct pathogenic effects in the host. This broader detection window for NS1 allows for extended evaluation of drug efficacy, beyond the short period when viremia is measurable. Moreover, a reduction in NS1 levels may not only indicate decreased viral replication but also suggest a potential reduction in disease severity due to its role in viral burden and pathogenicity. Utilising NS1 antigenemia as an additional surrogate marker for viral replication could enhance the ability to assess antiviral efficacy more comprehensively. While early treatment remains key to achieving maximal antiviral benefit, integrating NS1 measurements could provide a more practical and informative tool for evaluating antiviral candidates during clinical trials. Associate Professor Panisadee Avirutnan, Mahidol University, Thailand
Associate Professor Panisadee Avirutnan, Mahidol University, ThailandDr Avirutnan is a virologist specialising in dengue and flaviviruses. With a strong foundation in her graduate research on the dengue NS1 protein and its interaction with the human complement system, she expanded her focus during her postdoctoral fellowship at Washington University in St Louis to investigate NS1 proteins in other flaviviruses. Since 2010, she has been involved in the Division of Dengue Hemorrhagic Fever Research at Siriraj Hospital, where she contributes to clinical dengue cohorts and has participated in multiple investigator-initiated therapeutic trials. Currently, as the Director of SiCORE-DENGUE, she guides research aimed at identifying effective dengue therapeutics, understanding NS1 molecular mechanisms, and establishing the first controlled human dengue infection study in Thailand (DHIT). Through collaboration with local and international researchers, Dr Avirutnan is committed to advancing efforts to combat dengue and its associated challenges. 
Dr Junjie DingMahidol University, Thailand 
Dr Junjie DingMahidol University, Thailand Dr Junjie Ding received his PhD from Fudan University, China, in 2013. From 2016 to 2019 and again from 2023 to the present, he has worked as a pharmacometrics researcher Mahidol Oxford Tropical Medicine Research Unit (MORU) in Bangkok. Dr Junjie’s main research interest is model-informed drug development and dose-optimisation for treating infectious diseases, including malaria, tuberculosis, dengue fever, schistosomiasis, leishmaniasis and onchocerciasis. He primarily used population pharmacokinetic-pharmacodynamic and physiologically based pharmacokinetic (PBPK) modelling approaches to address critical clinical questions. Dr Ding has published over 40 papers in peer-reviewed journals. Before academia, Dr Ding served as the Head of the Clinical Pharmacology Department at AstraZeneca R&D China and as a team leader for PKS at Novartis R&D China, supporting the development of over 200 innovative drugs. |
| 16:00-16:15 |
Discussion
|
| 16:15-16:45 |
Rickettsial infections
Rickettsial infections have a global distribution and are transmitted to humans by ectoparasites such as ticks, mites, and fleas. Clinical presentations range from a mild febrile syndrome to, rarely, life-threatening sepsis or meningo-encephalitis. In Southeast Asia, species causing most human disease are Orientia tsutsugamushi and Rickettsia typhi. Accumulating evidence from clinical studies suggests doxycycline-based treatment regimens are optimal; however, defining suitable clinical endpoints for trials is challenging. Investigating the rate of bacterial killing in patients on different antimicrobials would improve our understanding of the therapeutic response. In Laos a randomised pharmacokinetic-pharmacodynamic study is underway to characterise clearance of Orientia tsutsugamushi and Rickettsia typhi from the blood of patients with scrub typhus or murine typhus treated with either doxycycline or azithromycin. Preliminary results of the rate of bacterial clearance estimated from serial qPCR measurements and clinical outcomes will be presented. 
Professor Elizabeth Ashley, Lao-Oxford- Mahosot Hospital-Wellcome Trust Research Unit, Laos

Professor Elizabeth Ashley, Lao-Oxford- Mahosot Hospital-Wellcome Trust Research Unit, LaosElizabeth Ashley is an Infectious Diseases Physician/ Microbiologist and Director of the Lao-Oxford-Mahosot Hospital-Wellcome Trust Research Unit in Vientiane. Her research interests include malaria, optimal treatment of infectious diseases in low-resource settings, antimicrobial resistance. |
| 16:45-17:00 |
Discussion
|
Chair

Professor Elizabeth Ashley, Lao-Oxford- Mahosot Hospital-Wellcome Trust Research Unit, Laos

Professor Elizabeth Ashley, Lao-Oxford- Mahosot Hospital-Wellcome Trust Research Unit, Laos
Elizabeth Ashley is an Infectious Diseases Physician/ Microbiologist and Director of the Lao-Oxford-Mahosot Hospital-Wellcome Trust Research Unit in Vientiane. Her research interests include malaria, optimal treatment of infectious diseases in low-resource settings, antimicrobial resistance.
| 09:00-10:00 |
Short talks
Modelling viral load kinetics during the COVID-19 pandemic: public health applications and lessons learned, Dr James Hay One of the most controversial topics during the COVID-19 was the implementation of occupational health testing programmes and guidelines for at-home testing to detect, isolate and release infectious individuals. Much of the evidence to guide these policies initially came from mathematical modelling studies in lieu of sufficient data on viral kinetics; a topic which saw little focus from infectious disease modellers prior to the pandemic. In addition, as the landscape of SARS-CoV-2 infection changed with new variants, immunity from vaccination and infection, and availability of antivirals, models and assumptions required constant updating. In this talk, James will give a brief overview of key mathematical modelling results and data on SARS-CoV-2 viral kinetics (timing, peak and variation of viral load following infection) and testing which he and others generated during the COVID-19. He will specifically focus on data from the USA National Basketball Association occupational health testing programme, which provided an unprecedented volume of longitudinal RT-qPCR testing data through the wildtype, Alpha, Delta and Omicron waves. Quantifying the time course of acute respiratory virus infections in this way has important implications for public health policies around screening, isolation, and surveillance, particularly in the context of vaccines and therapeutics. TREAT-GNB, a platform trial for severe Gram-negative bacterial infections , Dr Mo Yin Current clinical trial models for carbapenem-resistant Gram-negative bacterial (CRGNB) infections pose significant barriers to translation including overly stringent inclusion criteria that focus on limited types of infections, rigid randomisation treatment options, and a lack of access to patient cohorts at-risk of CRGNB infections. The ADVANCE-ID (Advancing Clinical Evidence for Infectious Diseases) network was jointly established by the Wellcome Trust, the University of Oxford, Mahidol University, Christian Medical College Vellore (CMC Vellore), and Singapore academic institutions to promote transnational research collaboration and capacity building for a sustainable pipeline to conduct large-scale clinical trials in infectious diseases. We challenge the existing paradigm with our platform trial, TREAT-GNB, which adopts a novel trial design: the Personalised RAndomised Controlled Trial (PRACTical) design. The main strength of the PRACTical design is a flexible randomisation list which tailors treatment based on individual patient requirements. Of all the regimens under consideration, study participants would be randomly assigned only to those regimens that were considered clinically reasonable for that patient at that time, incorporating antimicrobial susceptibility, toxicity profile, and physician judgement (ie using a personalised randomisation list). The set of patients with the same personalised randomisation list would then form the unit analogous to a trial in network meta-analysis. The design allows for existing antibiotic combinations to be included in the randomisation list, with potential to engage industry partners to add novel FDA- or European Medicines Agency-approved antibiotics to the randomisation lists, as they become available, so that they can be ranked against other regimens. Regimens will be ranked according to efficacy, resistance phenotype, safety and cost. In this talk, the speaker will introduce the PRACTical study design and its application for CRGNB infections. Influenza, Dr Phrutsamon Wongnak Viral respiratory infections represent a major global health threat, contributing significantly to morbidity and mortality, particularly in high-risk populations. Developing a robust pharmacodynamic framework to measure and compare the efficacy of antiviral agents is essential for informing intervention strategies aimed at mitigating the public health impact of these infections. This presentation outlines the use of adaptive open-label, phase 2, randomised controlled platform trials and the measurement of viral clearance rates, rather than time to PCR negativity, as a primary outcome in assessing antiviral efficacy. This approach is being applied to infections caused by SARS-CoV-2, influenza, and respiratory syncytial virus. Once randomised, daily serial oropharyngeal swab samples were collected from participants, and viral densities were measured daily using qPCR. A hierarchical Bayesian modelling framework was employed to estimate the viral clearance rate, defined as the slope of the log-linear decay in viral densities. The antiviral effect is defined as the relative change in the viral clearance rate among participants receiving treatment interventions compared to those who did not receive any treatment. Additionally, in infections with highly variable viral density dynamics over time, such as SARS-CoV-2, the impact of these temporal variations on head-to-head comparisons of antiviral efficacy and strategies for optimising sampling designs are discussed. A within-host model of chronic Trypanosoma cruzi infection to help inform drug and regimen selection, Miss Somya Mehra Trypanosoma cruzi is a kinetoplastid parasite causing Chagas disease, a major neglected tropical disease thought to affect over 6 million people worldwide. The current recommended treatment is 8 weeks of twice daily benznidazole, a regimen which is poorly tolerated in around a third of patients. There has been recent interest and funding in exploring intermittent treatment regimens and developing novel anti-parasitic drugs for T cruzi, with two candidates now in phase 1 trials. However, assessment of anti-parasitic efficacy in vivo for the treatment of chronic disease remains challenging. While correlates of blood-stage parasitaemia can be obtained using PCR methods, patients with chronic Chagas disease typically harbour very low parasite densities in the blood, close to the lower limit of quantification. Parasite biomass in the tissue additionally remains unobserved with current methods. In order to characterise the dose-response relationship for drugs against tissue stage and blood stage parasites, it is necessary to develop stochastic within-host models of T cruzi parasites. Multitype branching processes yield a natural theoretical framework to explore the cycling of T cruzi parasites between the bloodstream (trypomastigotes) and a tissue reservoir (amastigotes), including determinants of the steady state parasite burden; the probability of stochastic extinction at low parasite densities; and the potential consequences of drugs with differential effects on tissue and blood stage parasites. Interrogating simple models of T cruzi parasite clearance and replication can yield insights of practical value. Optimal Resource Allocation for Infectious Diseases, Dr David Price Design of experiments is not a new concept. However, much of the classical experimental design work was developed for the purpose of hypothesis testing, ie how many resources are required to ensure sufficient statistical power to test a formal hypothesis. In contrast, many disciplines of research, including discovery science and public health, are often more concerned with estimation of a quantity or learning about a system, rather than hypothesis testing. This talk will introduce the optimal design framework, a decision-theoretic approach to get the most information from the limited available resources. We will consider scenarios where the purpose is to either estimate parameters or discriminate between competing models as well as possible. Examples in each case will relate to learning about infectious disease dynamics. 
Dr James HayUniversity of Oxford, UK 
Dr James HayUniversity of Oxford, UK James is a research fellow at the University of Oxford Nuffield Department of Medicine funded through a Wellcome Trust Early Career Award. He completed his PhD at Imperial College London in 2019 and spent three years as a postdoc at the Harvard Chan School of Public Health. His expertise is in infectious disease modelling, with a specific interest in using quantitative biomarker data, such as viral loads and antibody titers, to understand and track the dynamics of infectious diseases, particularly influenza and SARS-CoV-2. He typically uses Bayesian multi-level models to link data and models across scales, from within-host models of viral kinetics and immune responses to agent-based models of disease spread. 
Dr Mo Yin, University of Singapore, Singapore

Dr Mo Yin, University of Singapore, SingaporeDr Mo Yin is an Infectious Diseases physician and a clinician scientist based at the National University Hospital, Singapore. Her research interest is in antimicrobial resistance and emerging infectious diseases. Driven by the ideal of using quality clinical research to improve patient outcomes and propel global policies, Dr Mo Yin designs and leads large multinational clinical trials which focus on pragmatic clinical solutions. In addition, Dr Mo Yin has expertise in mathematical modelling, statistics, bioinformatics and qualitative research. She is the deputy director of the ADVANCE-ID, a large clinical trial network consisting of over 60 hospitals globally. She has received numerous awards for her achievements in clinical care, research and teaching, and served as an external consultant to the World Health Organisation and Public Health England. Dr Mo Yin obtained her MBBS from the National University of Singapore and DPhil from the University of Oxford. 
Dr David Price, University of Melbourne, Australia

Dr David Price, University of Melbourne, AustraliaDr David Price is a Senior Research Fellow in the Department of Infectious Diseases and Melbourne School of Population and Global Health, at the University of Melbourne. His primary research interests are in the development and application of statistical methods for the study of infectious diseases, particularly regarding the optimal use of resources in experimental and observational investigations. He works on infectious diseases across multiple scales, from within-host infection dynamics to multi-site clinical trials and population-level epidemiological modelling and analysis. At the Doherty Institute, he is co-lead of the Computational Sciences and Genomics Cross-Cutting Discipline and leads a team providing collaborative statistical and modelling expertise to a breadth of infection and immunity research. Dr Phrutsamon WongnakMahidol Oxford Research Unit, Thailand Dr Phrutsamon WongnakMahidol Oxford Research Unit, Thailand Dr Phrutsamon Wongnak currently serves as a statistician for the PLATCOV trial and is an active member of the mathematical modelling group at the Mahidol Oxford Tropical Medicine Research Unit (MORU). With a background in veterinary medicine and a strong passion for public health, he is committed to advancing evidence-based decision-making and improving health policies, related to human, animal, and environmental health, through computational approach. His current projects primarily focus on assessing the effects of antivirals on accelerating viral clearance rates in randomised controlled trials, particularly for infections caused by SARS-CoV-2, influenza, and respiratory syncytial virus, contributing to more effective treatment strategies and interventions. 
Miss Somya Mehra, Mahidol Oxford Tropical Medicine Research Unit, Thailand

Miss Somya Mehra, Mahidol Oxford Tropical Medicine Research Unit, ThailandSomya has recently commenced a DPhil in the Nuffield Department of Medicine at the University of Oxford, focusing on mathematical models of chronic Chagas disease. Since late 2022, she has been based at the Mahidol Oxford Tropical Medicine Research Unit in Bangkok, where she has developed within-host models of relapse dynamics for vivax malaria, and classification models for falciparum malaria treatment failure. Prior to this, she had a placement at the Harvard School of Public Health as a Fulbright Future Scholar, working on the estimation of relatedness between malaria parasites. She completed her previous studies, including an MSc in Mathematics and Statistics, at the University of Melbourne, where she concurrently worked as a research assistant on stochastic and epidemic models of malaria. Professor David Price, Vice-Provost, Research, UCL
Professor David Price, Vice-Provost, Research, UCLDavid is Vice-Provost (Research) at UCL and Professor of Mineral Physics. David has an undergraduate degree and a PhD from the University of Cambridge. He was a Fulbright-Hayes Scholar and Research Associate at the University of Chicago, and a Research Fellow at Clare College Cambridge, before coming to UCL in 1983 as a Royal Society University Research Fellow. At UCL, he was appointed Professor at the age of 34, and later served as Head of the Department Earth Sciences, and as Dean of Mathematical and Physical Sciences, before being appointed to his current position of Vice Provost in 2007. He was one of the first to establish the now major interdisciplinary field of computational mineral physics, and has published over 230 research papers. He was awarded the Schlumberger Medal of the Mineralogical Society of Great Britain in 1999; the Murchison Medal of the Geological Society of London in 2002; and in 2006 he was awarded the Louis Néel Medal of the European Geosciences Union for "establishing the importance of computational mineral physics in Earth sciences and for outstanding contributions to the physics of the Earth’s core". He is a Member of the Academia Europaea and an Elected Fellow of the American Geophysical Union and of the Mineralogical Society of America. He has been an editor of Elsevier’s "Earth and Planetary Science Letters" (2005-8), and was President of the Mineralogical Society of Great Britain and Ireland (2004-6). He was a member of the UK’s HEFCE RAE2008 sub-panel on Earth and Environmental Sciences, and is now chair the REF2014 sub-Panel in this area. He is Chair of Governors of the UCL Academy School; a Council Member of the STFC; a non-executive Director the North Middlesex University Hospital NHS Trust; a Member of the Knowledge Advisory Group of the World Economic Forum; and a Member of Elsevier’s Academic Executive Advisory Board. |
|---|---|
| 10:00-10:30 |
Discussion
|
| 10:30-11:00 |
Break
|
| 11:00-11:30 |
Bridging the gap: pharmacokinetic-pharmacodynamic modelling to optimise antimalarial dosing
The success of malaria control relies on the availability of highly effective antimalarial drugs. The widespread emergence of drug-resistant parasites now threatens the efficacy of first-line treatments, necessitating the urgent development of novel regimens and combinations of existing and new therapeutic agents to ensure adequate cure of malaria. To addressing this challenge, mechanistic within-host models that integrate the blood antimalarial drug concentrations with the parasite-time profile (also known as antimalarial pharmacokinetic-pharmacodynamic (PK-PD) models), provide a valuable decision tool for determining optimal antimalarial dosing regimens. This presentation will provide an overview of published antimalarial PK-PD models, highlighting the differences in the mechanistic structure to capture malaria biology, and the relationship between drug concentration, drug-drug interaction and pharmacodynamic effect. Additionally an evaluation of the statistical approaches used for model validation against clinical data will be described, and a three step framework for the development and evaluation of PK-PD models recommended. 
Professor Julie Anne Simpson, University of Melbourne, Australia

Professor Julie Anne Simpson, University of Melbourne, AustraliaProfessor Julie Simpson is Head of Biostatistics at the Melbourne School of Population and Global Health and Director of the Methods and Implementation Support for Clinical and Health research (MISCH) Hub at the University of Melbourne, and a Visiting Professor of the University of Oxford. She has 30 years’ experience collaborating on multidisciplinary research projects with clinicians, laboratory scientists, epidemiologists and health policy-makers at universities and hospitals worldwide, and has published >370 papers. Her main area of research is the integration of biostatistics and mathematical modelling to improve the control of infectious diseases. |
| 11:30-11:45 |
Discussion
|
| 11:45-12:15 |
Opportunities for therapy in Chikungunya infection
Chikungunya is an arboviral infection whose clinical presentation is very similar to those of dengue and zika. Fever occurs in the great majority of individuals and viremia is measured in all patients till 72 hours of the beginning of symptoms. Viral decay is homogeneous and most individuals are negative at 4 days after they are first seen. Although most symptoms are limited to the first days of infection, at 7-9 months after infection, 50% of patients who had chikungunya still reported some degree of discomfort and 25% needed to take some kind of pain killer to decrease symptoms. In patients with Chronic Chikungunya infection, there are 3 major clinical syndromes: (i) Rheumatoid arthritis-like; (ii) Spondyloarthropathy-like and (iii) fibromyalgia-like syndromes. This classification of clinical presentation is useful for therapeutic purposes and follow-up of patients. Most individuals report their disease is significantly better at 18 months after infection. Experimentally, Chikungunya virus infection of mice is associated with transient viremia and viral infection of the site of infection and significant persistent inflammation and TNF expression at the dorsal root ganglia that innervates the infective site. These studies show that the viremia that follows chikungunya infection is high and has a kinetics compatible with the testing of antiviral compounds. In participants, with chronic infection, aggressive anti-inflammatory and pain management is needed for return to normal activities, especially because there is much impact on quality of life and the disease tends to very limited in duration. 
Professor Mauro Martins Teixeira, Federal University of Minas Gerais, Brazil

Professor Mauro Martins Teixeira, Federal University of Minas Gerais, BrazilMauro Teixeira is professor of Immunology at the Federal University of Minas Gerais (UFMG). His MD if from UFMG and PhD from the University of London. He works with inflammation in the context of infectious and chronic inflammatory diseases. His group has provided extensive preclinical and more recently clinical evidence that anti-inflammatory drugs may be useful as adjunct treatment of infectious diseases. He has collaborated extensively with the Brazilian effort to design trials and evaluate strategies to control arboviruses, including vector and vaccine trials. He participates in several relevant international cooperations, including CERCLE (Coalition for Equitable ResearCh in Low-rEsource settings), DNDI-Dengue Alliance, PlatCOV (with MORU Tropical Health in Thailand) and Coordinating Research on Emerging Arboviral Threats Encompassing the Neotropics (CREATE-NEO, with UTMB). He is president of the International Association of Inflammation Societies. |
| 12:15-12:30 |
Discussion
|
Chair
Professor Nick White FRS, Mahidol Oxford Research Unit
Professor Nick White FRS, Mahidol Oxford Research Unit
Professor Nick White is Professor of Tropical Medicine at the Faculty of Tropical Medicine, Mahidol University, Thailand and Oxford University, UK. He is a Wellcome Trust Principal Research Fellow who chairs the Wellcome Trust Tropical Medicine Research Programmes in South East Asia. His main research focus is the pathophysiology and treatment of malaria. He also currently conducts pharmacometric research on COVID-19, influenza, and Chagas disease. Professor White has received the Prince Mahidol Prize for Medicine, the Canada Gairdner Foundation Global Health Prize, and the Royal Society of Tropical Medicine and Hygiene Manson medal. He has been a member of the WHO antimalarial treatment guidelines committee for 20 years (and co-chaired it for twelve) and he currently chairs the Scientific Advisory Committee of the Drugs for Neglected Diseases initiative and the Coalition for Equitable Research in Low Resource Settings.
| 13:30-14:00 |
Reductio ad unum: the single patient RCT
Pharmacometric studies allow for greater efficiency in determining effects which translate to smaller sample sizes. Certain rare diseases with particular profiles, and particular drugs, discussed in this talk, may allow for sample sizes of 1. Dr William Schilling, Mahidol Oxford Tropical Medicine Research Unit, Thailand
Dr William Schilling, Mahidol Oxford Tropical Medicine Research Unit, ThailandWill is a an Infectious Diseases/ Microbiology Registrar working at St George’s Hospital London and was a research physician working at the Mahidol Oxford Tropical Medicine Research Unit (MORU) prior to this. At the time of reading this biography he may or may not now have a DPhil. Will’s work at MORU focussed on COVID-19. This was initially a large multinational prophylaxis study of hydroxychloroquine/ chloroquine but as the pandemic progressed, a platform pharmacometrics study assessing various therapeutics in early treatment- PLATCOV. Subsequently, Will has been involved in similar studies in influenza, RSV and dengue. Will has previous experience working in Medicine in Mbarara, Uganda. He hopes to one day do a 5K or 10K fun run. |
|---|---|
| 14:00-14:15 |
Discussion
|
| 14:15-14:45 |
Perspective on PK/ PD and QSP modelling for anti-infective drug discovery and development

Suzanne Gaudet, Novartis Institutes for Biomedical Research, USA

Suzanne Gaudet, Novartis Institutes for Biomedical Research, USASuzanne Gaudet co-leads the Translational Modeling group in Pharmacokinetics Sciences (PKS) at Biomedical Research, Novartis. While the group’s work touches all modalities and disease areas, Suzanne’s primary responsibilities are in Global Health, Oncology, and Predictive Safety. Suzanne earned a PhD in Biochemistry from Harvard University and did her postdoctoral research at MIT. From 2003 to 2008, she worked as a research scientist and scientific coordinator at the Cell Decision Processes Center at MIT and Harvard. Prior to joining Novartis in 2019, Suzanne was an assistant professor in Genetics at Harvard Medical School and the Dana-Farber Cancer Institute. Her federally funded research group focused on understanding how signalling responses to TNF superfamily ligands influence different cell fates (apoptosis, differentiation, response to infection) using a systems biology approach. |
| 14:45-15:00 |
Discussion
|
| 15:00-15:30 |
Break
|
| 15:30-16:00 |
Regulatory perspective
Regulatory agencies have been adjusting their requirements for early clinical development of anti-infective agents, taking into account scientific advances in the area of PK/ PD so make dose finding studies as efficient as possible. PK/ PD evaluations are considered now standard practice for antibacterial medicines. Proper preclinical evaluation of PK/ PD together with Phase I PK and safety data could allow skipping formal dose finding studies in the context of antibacterial agents development. In other areas, clinical trial to select appropriate doses for confirmatory clinical trials are still needed. Surrogate endpoints based on a pharmacodynamic marker could be considered based on the level of confidence that has been gathered with respect to specific microbiological evaluations, eg viral loads measurement in upper respiratory tract for new antivirals for respiratory viruses. More work is needed to advance translational medicine that could increase the efficiency of clinical development for new treatments for infectious diseases. Dr Marco Cavaleri, European Medicines Agency, Netherlands
Dr Marco Cavaleri, European Medicines Agency, NetherlandsMarco Cavaleri is Head of Department, Public Health Threats. He is the Chair of EMA Emergency Task Force (ETF) and responsible for EMA activities for emergent pathogens, vaccines and AMR. He serves in different advisory groups at WHO, including PDVAC, AMR priority pathogens and R&D Blueprint SAG and clinical trials working group. Marco Cavaleri is a Pharmacologist who spent several years in industry in R&D mainly in the area of anti-infectives covering different positions in preclinical and clinical development of new antibacterial, antitubercular and antifungal agents. He has expertise in microbiology, animal models, PK/ PD and clinical trial design for antibacterial and TB drugs, from early phase to late stage clinical trials. He is involved in several areas of vaccines and innovative therapies development, such as bacteriophages, that could tackle AMR. He has been driving the EMA AMR strategy on human medicines since 2009 including the international partnerships that lead to alignment of clinical trials requirements for new antibacterial agents with FDA, PMDA and HC. He is co-author of several publications related to AMR, TB, antibiotics, vaccines, and phages. |
| 16:00-16:15 |
Discussion
|
| 16:15-17:00 |
Panel discussion and overview
|
